.webp)
Food allergy testing is how we figure out precisely which foods are causing your immune system to overreact. It's a methodical process, using clinically proven techniques to identify the specific proteins that trigger your symptoms. For so many people, it's the first real step towards getting back in control and leaving the fear of a reaction behind.
Think of your immune system as your body's personal security detail. Its main job is to spot and deal with genuine threats like viruses or harmful bacteria. But with a food allergy, that system gets its wires crossed. It mistakenly flags a harmless food protein—from something like milk, eggs, or nuts—as a dangerous invader.
Once that mistake is made, the immune system launches a full-blown counter-attack. It releases specific antibodies known as Immunoglobulin E (IgE), which are basically alarm bells. These IgE antibodies latch onto certain cells, instructing them to unleash a flood of chemicals like histamine. This chemical release is what causes the classic allergy symptoms we all recognise, from hives and swelling to breathing difficulties.
The whole point of food allergy testing is to play detective and pinpoint exactly which food proteins are setting off those IgE alarms. It helps doctors confirm whether your symptoms are the result of a genuine allergy or something else entirely.
Making this distinction is absolutely crucial. It separates a potentially life-threatening immune response from other, less severe conditions. For instance, it's very common for people to mix up food allergies with food intolerances.
Getting a confirmed diagnosis through proper testing gives you a clear roadmap. It stops the guesswork, prevents you from cutting out foods unnecessarily, and gives you the knowledge to avoid your triggers and know what to do in an emergency.
Understanding how your body reacts is more important today than ever before. Food allergy rates in the UK have become a significant public health issue. A recent analysis of UK population data showed that among young children aged 3–4, food allergy rates were as high as 9.1%. That means almost one in ten young children could be affected, which really underlines how vital reliable testing and management are.
While our focus here is on food, it's worth remembering that many people also deal with other common allergies from environmental factors. Broadening your knowledge by understanding different allergy triggers like pet dander can sometimes provide helpful context. At the end of the day, though, professional testing is the only way to get a clear and accurate diagnosis, making sure you get the right advice and care.
When it comes to pinpointing a food allergy, guesswork just won't cut it. To get a reliable answer, allergists use a specific set of medically validated tools. These methods are all about accurately identifying how the immune system responds to certain food proteins, moving beyond symptoms alone to get to the biological root of the problem.
Think of your allergist as a detective. They gather initial clues from your medical history and symptom diary, but then they need hard evidence to confirm their suspicions. This evidence comes from scientifically proven tests trusted by medical professionals worldwide. Let’s break down the three main methods used in clinical practice.
This infographic helps visualise the crucial difference between a true allergy, which involves the immune system, and an intolerance, which is a digestive issue.
The key thing to remember is that clinically proven tests are designed to detect the immune system's allergic response, not the digestive symptoms linked with an intolerance.
To give you a clearer picture, here’s a quick comparison of the validated tests we’ll be discussing.
Each test provides a different piece of the puzzle, helping your allergist build a complete and accurate picture of your condition.
The Skin Prick Test (SPT) is one of the most common and fastest ways to test for a food allergy. It’s a frontline diagnostic tool that delivers results in about 15-20 minutes, giving your allergist immediate insights.
During an SPT, a tiny drop of liquid containing a specific food allergen is placed on your skin, usually your forearm or back. A small, sterile lancet then gently pricks the skin’s surface through the drop. It’s not painful—most people say it feels like a light scratch. The idea is to introduce a minuscule amount of the potential allergen to the immune cells just under the skin.
If you're allergic to that substance, your immune system flags it as a threat and releases histamine. This causes a small, raised, itchy bump to appear, much like a mosquito bite. This reaction is called a wheal, and its size is measured by the clinician. Generally, a larger wheal suggests a higher chance of an allergy.
Another cornerstone of allergy diagnosis is the Specific IgE (sIgE) Blood Test. While a skin prick test checks for a reaction on your skin, this blood test looks for evidence in your bloodstream. Think of it as a highly specific detective, hunting for the IgE antibodies your immune system has created to fight off a particular food protein.
Here’s how it works:
The results come back as a numerical value, showing the concentration of these antibodies. A higher level often correlates with a greater probability of a clinical allergy. This method is especially useful for people who can't have a skin prick test, perhaps due to a skin condition like eczema or because they’re taking medications that would interfere with the results. To learn more about how lab analysis plays a role in healthcare, you can explore the different types of private blood testing services in the UK.
Important Takeaway: Both the skin prick test and the IgE blood test detect sensitisation. This simply means your body has produced IgE antibodies to a food. However, sensitisation is not the same as a clinical allergy. It’s a vital clue, but it doesn't automatically mean you'll have a reaction when you eat the food.
Finally, we have the most definitive method: the Oral Food Challenge (OFC). This is considered the 'gold standard' for allergy diagnosis because it directly answers the ultimate question: will eating this food actually cause an allergic reaction? Because of the potential for a severe reaction, this test is always done in a medical setting under strict supervision.
During an OFC, you’re given very small, gradually increasing amounts of the suspected food allergen over several hours. The whole time, the medical team watches you closely for any signs of a reaction.
If you develop any allergic symptoms, the challenge is stopped immediately, and you're given medication if necessary. A successful OFC, where you eat the full portion without a reaction, definitively rules out that food allergy. On the other hand, a reaction during the challenge confirms the diagnosis. It’s the ultimate way to separate simple sensitisation from a true, clinical allergy.
Getting clear, accurate results from your food allergy testing appointment starts long before you ever step foot in the clinic. Think of yourself as a detective gathering clues; the better the information you bring, the faster your allergist can crack the case.
Proper preparation is what makes your tests effective and your consultation genuinely productive. By taking a few simple but vital steps beforehand, you give your specialist the detailed insights they need to connect your symptoms to potential triggers. It’s all about making sure that time with them is as valuable as it can be.
Your own experience is probably the most powerful diagnostic tool we have. A food and symptom diary creates a running record that helps both you and your doctor spot patterns that would otherwise be completely missed. For at least one to two weeks before your appointment, track everything you eat and how you feel with as much detail as you can muster.
Your diary should include:
This log gives your allergist crucial clues, helping them narrow down the potential culprits and decide exactly which allergens to test for.
This step is absolutely critical, particularly if you're coming in for a skin prick test. Antihistamines, the go-to for allergy symptoms, work by blocking the very chemical reactions the skin test needs to measure. Taking them before your test can easily lead to a false-negative result, meaning a genuine allergy could be missed.
Imagine trying to test a smoke alarm while the batteries are out. No matter how much smoke fills the room, the alarm won't sound. Antihistamines do something similar to a skin prick test—they temporarily disable the 'alarm' your skin would normally trigger.
Your clinic will give you specific instructions, but as a general rule, you should plan to stop taking antihistamines for 3-7 days before your appointment. This includes a lot of over-the-counter hay fever, cold, and even some sleep medications. Always check with your allergist for a precise timeline and a full list of medications to avoid. Crucially, do not stop taking any prescribed medications without direct medical advice.
Knowing what’s going to happen can help you feel much more relaxed and prepared. Your appointment will be a two-way conversation, focused on piecing together your health history and your recent symptoms.
A typical consultation involves:
Being prepared helps the whole process run smoothly. For a complete overview of what to expect as a new patient, our guide on allergy and intolerance testing information is a great place to start.
Getting your food allergy testing results can feel like you've finally found the missing piece of the puzzle. But seeing a "positive" result on paper can also be confusing, or even a bit scary. It's crucial to understand that a positive test isn't a final verdict; it's a vital clue that needs an expert eye to interpret correctly.
The results from a skin prick test or an IgE blood test reveal sensitisation, not necessarily a clinical allergy. This is one of the most important distinctions in allergy care, and it’s where a lot of confusion comes from.
Simply put, sensitisation means your immune system has created IgE antibodies in response to a specific food protein. That’s it.
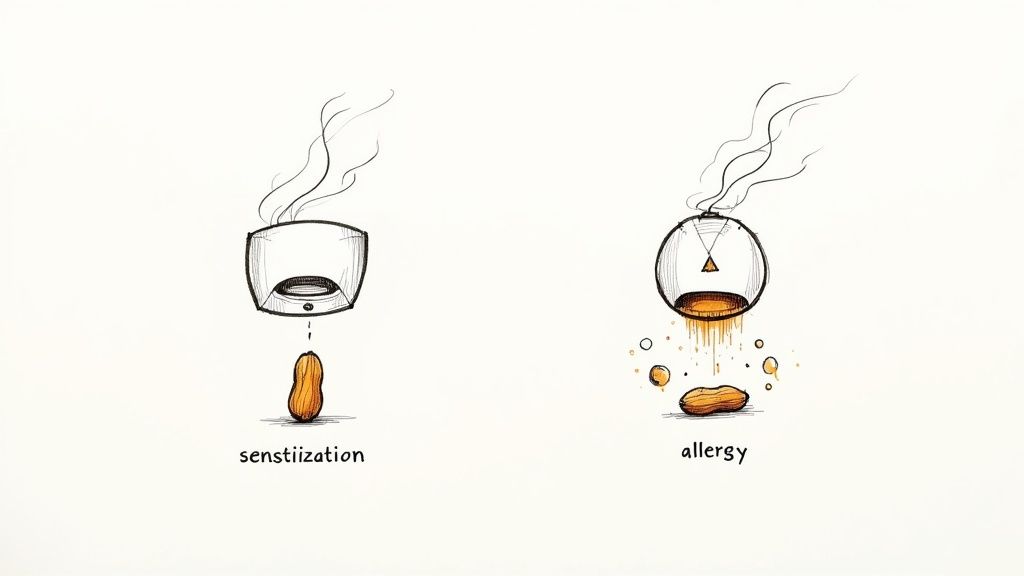
Think of sensitisation like installing a smoke alarm in your home. The alarm is now in place and could go off, but it only signals a real problem when there's actual smoke.
In this analogy, the IgE antibody is the smoke alarm, and the allergic reaction you experience after eating the food is the smoke. Just because the alarm is there (sensitisation), doesn’t mean it will definitely go off. A true clinical allergy is only confirmed when that sensitisation is paired with a consistent history of symptoms whenever you’re exposed to the food. An allergist is the only one who can properly connect these dots.
A positive test result in someone who has never had a reaction to that food does not diagnose a food allergy. It only indicates a potential risk, which must be evaluated in the context of your complete medical history.
This is exactly why self-diagnosing based on test results is so risky. It can lead to unnecessary dietary restrictions, nutritional gaps, and a huge amount of stress.
A big question we often hear is whether the size of the skin test reaction or the IgE level in a blood test predicts how severe an allergic reaction might be. The short answer is: generally, no.
While a larger wheal on a skin prick test or a higher IgE level can increase the likelihood that you have a genuine allergy, it doesn't tell us anything about the potential severity of a future reaction. Someone with a small reaction could still have a severe, life-threatening response, while another person with a very large reaction might only ever get mild hives.
This is a critical point. The main goal of these tests is to identify the trigger, not to grade the danger. Your allergist uses this information alongside your personal history to build the complete picture.
Interpreting food allergy test results is a specialised skill. Your allergist acts like an expert detective, combining the hard evidence from your tests with the story you provide from your food and symptom diary.
They will consider several key factors:
For children, this careful interpretation is especially vital. A specialist paediatric dietitian can give expert guidance on how to manage a child’s diet safely after a diagnosis, making sure they get all the nutrients they need to grow. You can find more information about how a paediatric dietitian can support your family's needs on our services page.
Ultimately, your results are just one part of a bigger diagnostic process. They provide scientific data, but that data is only meaningful when it's filtered through clinical expertise and your unique personal experience.
After getting to the bottom of your results, you may need to adjust your diet. Navigating this new landscape can be a challenge, but resources for finding safe gluten-free and nut-free snacks can be incredibly helpful for managing day-to-day life. A confirmed diagnosis is the first step towards creating a safe and confident lifestyle.
Figuring out how to get reliable food allergy testing in the UK is the first step towards a diagnosis you can trust. Thankfully, there’s a clear pathway to specialist care, designed to guide you towards evidence-based advice and protect you from unproven methods.
For most of us, the journey starts with a trip to the local GP. This should always be your first port of call for any health concern, especially suspected allergies. Your GP will take the time to listen to your story, go over your symptoms, and do an initial check. If they suspect a food allergy is at play, they’ll refer you to a specialist NHS allergy clinic.
Once you get that referral, you’ll be in the hands of an allergist or immunologist—doctors who’ve spent years training to diagnose and manage allergic conditions. This specialist-led approach is non-negotiable, because as we've already covered, making sense of test results is a real skill. It means your diagnosis is based on the full picture, not just one isolated lab report.
The process usually unfolds like this:
It's not just about the clinics. Your safety is also backed up by some pretty robust regulations. The UK’s Food Standards Agency (FSA) is a key player here, mandating clear labelling for the 14 major allergens. This law forces food producers to be upfront about common triggers like nuts, milk, and gluten on their packaging. It’s a game-changer for anyone with an allergy trying to do their weekly shop safely.
But making sure those labels are accurate takes constant work. A review commissioned by the FSA recently flagged some gaps in the allergen testing protocols used across the industry. It pointed out that some common tests aren't always reliable and that certain allergenic proteins can become impossible to detect after cooking, which is a real risk. You can learn more about the FSA's findings on allergen testing and what they're recommending to fix it.
This two-pronged approach, combining healthcare pathways and food safety laws, creates a supportive environment. It gives you the confidence to seek out proper medical care and to trust the food labels you depend on.
While the NHS provides fantastic care, we all know that waiting times for specialist appointments can be long. For anyone looking for faster answers and a management plan, exploring private allergy testing can be a sensible alternative. It often means quicker consultations and a more personalised care plan. By understanding both the NHS and private routes, you can make the right call for your family.
When you're struggling with symptoms and desperate for answers, it’s all too easy to be lured by tests promising a quick fix. The internet is flooded with them. But the world of allergy diagnosis is full of methods that simply don’t have the science to back them up. You need a healthy dose of scepticism to avoid wasting your money—and more importantly, to avoid a harmful misdiagnosis.
The demand for answers has created a booming market. In fact, the UK allergy diagnostics market is projected to hit USD 502.1 million by 2030, fuelled by the sheer number of adults and children affected by allergies. Unfortunately, this high demand also means that unproven methods can thrive by targeting people who are just looking for help. You can read more about the UK allergy diagnostics market growth and what’s driving it.
Think of these tests as a faulty compass; they’ll point you in a direction, but it's not one you can trust with your health. Following their advice can lead to cutting out essential foods for no reason or, worse, a dangerous false sense of security.
Several popular tests are not recommended by the NHS or leading organisations like Allergy UK because they simply aren't scientifically validated for diagnosing true food allergies.
Here are a few of the most common ones to watch out for:
It is crucial to remember that these alternative tests do not measure the IgE-mediated response that defines a true food allergy. Their results are unreliable and should not be used to make decisions about your diet or health.
Choosing a scientifically validated test isn't just about getting an accurate result; it’s about keeping you safe. An incorrect diagnosis from one of these unproven tests could lead you to avoid a whole range of nutritious foods, potentially causing deficiencies without any real benefit.
Even more dangerously, it might give you a false all-clear, causing you to overlook a genuine, serious allergy. For a reliable diagnosis, it’s essential to stick with methods that are clinically proven and interpreted by a specialist. Our guide on the combined allergy and intolerance test explains the validated approaches used in clinical practice.
Always consult a healthcare professional for advice on food allergy testing.
It’s completely normal to have questions when you’re trying to get to the bottom of a suspected food allergy. The whole process can feel a bit overwhelming, so let's clear up some of the most common queries we hear.
Getting straight answers helps take the mystery out of testing and lets you have a much better chat with your specialist. Think of this as filling in the gaps, so you can move forward with confidence.
This really comes down to the type of test used and, crucially, how the results are interpreted by an expert. The most common methods, like skin prick tests and IgE blood tests, are great at identifying sensitisation—which is just a technical way of saying they can spot the allergy antibodies in your system.
But here’s the key thing to remember: they can throw up false positives. A positive test proves your immune system has noticed a food, but it doesn't automatically mean you'll have a reaction when you eat it. That's why your own history of symptoms is so vital to the diagnosis.
The most reliable test we have is the Oral Food Challenge (OFC). It’s considered the 'gold standard' because it involves eating the food in a controlled, medically supervised setting. It’s the only way to see what actually happens, confirming or ruling out an allergy for good. A proper diagnosis always combines your story with the test results, all pieced together by an allergist.
Absolutely. You can suddenly develop an allergy to something you’ve eaten your entire life without a problem. It’s known as adult-onset food allergy, and we’re seeing it more and more often.
Shellfish is a classic culprit for new allergies in adults, but honestly, it can happen with any food. We don’t fully understand why, but it seems to be linked to changes in our immune system or environment over time. If you suddenly start getting hives, swelling, or an upset stomach after eating a particular food, it’s definitely worth a chat with your GP.
This is a really important one to get straight. A food allergy is a full-blown immune system response. Your body mistakenly flags a protein in food as a dangerous invader and releases chemicals like histamine to fight it. This is what causes symptoms ranging from mild itchiness to life-threatening anaphylaxis.
A food intolerance, however, has nothing to do with your immune system. It’s usually a digestive problem. Lactose intolerance is a perfect example—the body just doesn't have enough of the right enzyme to break down milk sugar. The symptoms, like bloating, gas, or diarrhoea, are uncomfortable but not life-threatening. The medical tests we've discussed are designed to diagnose true immune-related allergies only.

