.webp)
An inguinal hernia repair is a routine operation to fix a bulge in the groin. The bulge itself is usually a bit of tissue, like fat or even part of the intestine, that has pushed through a weak spot in the abdominal wall. It's one of the most common surgeries performed in the UK, designed to get rid of the discomfort and stop any serious problems from developing down the line.
Think of your abdominal wall as a strong, multi-layered sheet of muscle and tissue. It's designed to hold everything in. But sometimes, a weak spot or a small tear can develop. An inguinal hernia is what happens when something from inside—usually fatty tissue or a loop of intestine—pokes through that weak spot.
This creates a noticeable lump in the groin. It's not just a cosmetic issue; it's a structural failure. Everyday actions like coughing, lifting something heavy, or even straining on the toilet can force more tissue through the gap, making the bulge bigger and more painful.
While some hernias don't cause any pain at all, many lead to a persistent ache, a feeling of heaviness, or even sharp pains, especially when you're on your feet or being active.
Inguinal hernias usually happen because of two things working together: a pre-existing weak spot in your abdominal wall and an increase in pressure inside your abdomen.
Some of the most common culprits include:
The most obvious sign is that bulge in your groin or scrotum. You might notice it disappears when you lie down and comes back when you stand up. You might also feel a dull ache that gets worse as the day goes on. If you're getting these kinds of symptoms, it's worth understanding the other common causes of groin pain, too.
It can be tempting to ignore a hernia if it isn't causing much bother, but leaving it can lead to a very serious complication called strangulation. This is when the tissue that's poking through gets trapped and its blood supply is cut off.
Strangulation is a medical emergency. It triggers sudden, severe pain, nausea, and vomiting. If it's not treated right away, the trapped tissue will die, leading to life-threatening infections and the need for much more complex, emergency surgery.
This risk is why surgeons almost always recommend a repair. It's a definitive fix that closes the weak spot and stops these dangerous complications before they can happen.
The procedure is incredibly common. In fact, NHS England data shows that 87,651 inguinal hernia repairs were performed in a single year, making it one of the most frequently performed general surgical operations in the country. Getting it fixed isn't just about dealing with today's symptoms—it's about protecting your long-term health.
When it comes to inguinal hernia repair, your surgeon will likely talk you through two main surgical approaches. Think of it as choosing between two different routes to the same destination; both get the job done, but the journey and recovery can look a little different. The two primary methods are the traditional open repair and the more modern laparoscopic repair, which you might hear called keyhole surgery.
Each technique comes with its own set of advantages and is better suited to different patient circumstances. Getting to grips with how they work is the first step towards having a really productive conversation with your surgeon about which path is right for you. They'll recommend the best option based on your hernia's specifics, your general health, and your medical history.
Open inguinal hernia repair is the classic, time-tested method that surgeons have perfected over many decades. It’s seen as a highly reliable and effective procedure and can be performed under local, spinal, or general anaesthesia.
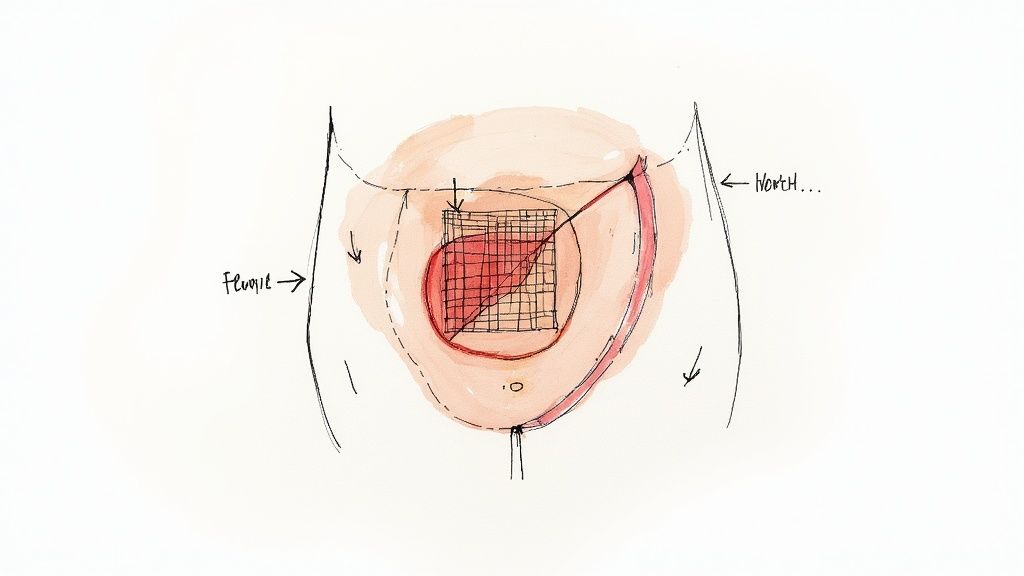
The process itself is quite straightforward. The surgeon makes a single incision, usually around 3 to 4 inches long, directly over the hernia in your groin. This gives them a clear, direct view of the hernia. They then gently push the protruding tissue back into the abdomen where it belongs. The final, and most crucial, step is to reinforce the weakened spot in the abdominal wall, almost always with a piece of surgical mesh to stop the hernia from coming back.
This infographic gives a simple guide on when to see a doctor about a potential bulge in your groin.
As the image shows, the presence of a groin bulge is a key sign that it's time to get a professional medical opinion.
Laparoscopic inguinal hernia repair is a more recent technique that is minimally invasive. This approach always requires general anaesthesia, as your abdominal muscles need to be completely relaxed for the surgeon to work safely.
Instead of one larger cut, the surgeon makes three tiny incisions, often less than half an inch each. A thin tube with a tiny camera on the end (a laparoscope) is inserted through one of these, giving the surgeon a magnified, high-definition view of the hernia from inside the abdomen on a monitor. Specialised surgical tools are then passed through the other small incisions to carry out the repair.
Just like in an open repair, the surgeon pushes the herniated tissue back into place and secures a piece of surgical mesh over the weak spot. The key difference is that the entire operation is done internally, from behind the abdominal wall.
This method is often the go-to for certain situations, such as when a patient has hernias on both sides (bilateral hernias) or if a previous open repair has failed and the hernia has returned.
To make the differences clearer, here's a side-by-side comparison:
FeatureOpen Hernia RepairLaparoscopic Hernia RepairIncision TypeOne larger incision (3-4 inches)Three small incisions (<0.5 inches each)AnaesthesiaLocal, spinal, or generalGeneral anaesthesia always requiredProcedure ViewDirect, external view of the herniaInternal view via a camera (laparoscope)Post-Op PainGenerally more discomfort immediately afterOften less pain reported by patientsRecovery TimeSlower return to normal activitiesFaster return to light activities and workScarringOne more noticeable scarMinimal, less visible scarsBest ForFirst-time hernias, very large hernias, patients who can't have general anaesthesiaRecurrent hernias, bilateral hernias, patients wanting a quicker return to activity
As you can see, the choice isn't about which one is "better" overall, but which is better for you.
Choosing between open and laparoscopic surgery means balancing the benefits and drawbacks of each. There really is no single "best" option; the ideal choice is always patient-specific. Navigating these options is often simpler with expert guidance, and understanding the benefits of seeking private medical care for surgery can provide clarity on accessing specialists who can offer personalised recommendations.
Key benefits of laparoscopic repair often include:
However, open repair is still an excellent and often preferred choice for good reason.
Reasons a surgeon might recommend open repair:
Ultimately, the goal of any inguinal hernia repair is a safe, durable fix that gets rid of your symptoms and lets you get back to your life. Your surgical team will thoroughly assess your situation and discuss their recommendation with you, making sure the chosen method aligns perfectly with your health needs and leads to the best possible outcome.
When a surgeon repairs a hernia, they're dealing with a weak spot in the abdominal wall. Just stitching the muscle back together is like trying to patch a hole in old, frayed fabric – the original material is already compromised, so the repair is under constant tension and at risk of tearing again.
This is where surgical mesh has completely changed the game in modern inguinal hernia repair.
Think of surgical mesh as a specialised scaffold or a high-tech patch. It’s a sterile, flexible sheet made from biocompatible synthetic materials, engineered to be both strong and lightweight. Instead of just pulling weakened tissues together under strain, the surgeon places this mesh over the hernia defect, creating a tension-free repair.
This approach fundamentally alters the healing process. The mesh gives immediate structural support, bridging the gap and taking the strain off the surrounding muscle. It’s this simple but effective principle that leads to a more durable, long-lasting fix.
Once it’s in place, the surgical mesh doesn't just sit there. It acts as a framework, encouraging your body's natural healing response. Over the weeks and months after your surgery, your own connective tissues, rich in collagen, grow into and around the tiny pores of the mesh.
This process, known as tissue integration, effectively incorporates the mesh into the abdominal wall itself. You’re left with a new, reinforced layer of tissue that’s significantly stronger than the original, weakened muscle could ever be on its own. It's a clever partnership between modern surgical technology and your body's own ability to heal.
The primary goal of using mesh is to drastically reduce the chance of the hernia coming back. By creating a robust, integrated repair, the mesh provides a permanent solution to the underlying weakness in the abdominal wall.
This method has become the cornerstone of successful hernia surgery because it works. Its use is now incredibly common. A large-scale analysis of NHS England data showed that nearly 19 out of every 20 inguinal hernia repairs now use mesh, making it the standard of care in the UK. You can find more details in the full population-based study.
The widespread use of mesh isn't an accident; it’s backed by decades of clinical evidence showing far better results than non-mesh (suture-only) repairs. The most important benefit is the dramatic reduction in the hernia coming back.
Here’s a quick look at the key advantages that make mesh the preferred choice:
Surgical methods are always being refined to improve these outcomes even further. To find out more about how surgical technology is evolving, have a read of our guide on the latest advancements in surgical techniques.
Ultimately, using surgical mesh in an inguinal hernia repair is all about creating strength and durability. It transforms the procedure from a simple patch-up job into a long-term structural reinforcement, giving you the best possible chance for a successful, permanent recovery.
Having inguinal hernia repair surgery is a massive step towards getting your life back. But the operation itself is only half the story. Knowing what to expect during your recovery is just as crucial for a smooth, successful outcome.
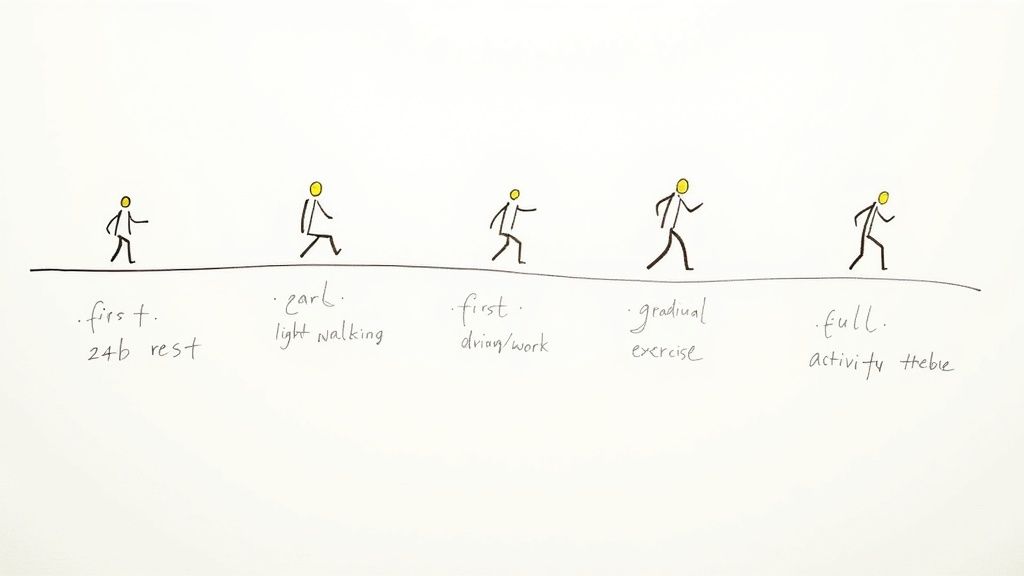
Think of your recovery as a journey with clear milestones. It’s a gradual process that takes you from the operating theatre right back to your everyday routine. While everyone heals at their own pace, this timeline gives you a solid roadmap for what lies ahead.
The first day is all about rest and managing any initial discomfort. Whether you’ve had open or keyhole surgery, you’ll likely feel sore and tired as the anaesthetic wears off. Don’t worry; your surgical team will make sure you have pain relief to keep you comfortable.
Most inguinal hernia repairs in the UK are now done as day-case procedures, which is a big shift towards faster, less invasive care. Research shows that day-case repairs jumped from 64% in 2016 to 78% in 2020—a huge change for a procedure performed over 70,000 times a year in the UK.
This means you’ll probably be heading home the same day. It’s essential to have a responsible adult stay with you for at least the first 24 hours.
Your main priorities are simple:
Over the first week, you should start to feel a little better each day. It’s completely normal to have some pain, swelling, and bruising around the groin and even the genital area.
Your pain should become much more manageable, and you might find you can switch from stronger prescription painkillers to over-the-counter options like paracetamol. A common post-surgery issue is constipation, and straining is the last thing you want. Your surgeon will likely recommend a high-fibre diet and plenty of fluids to keep things moving.
Recovery Tip: When you cough, sneeze, or get up, try holding a small pillow or your hand over the incision site. This simple trick can make a huge difference in reducing discomfort and that pulling sensation on the stitches.
You’ll also need to keep the wound clean and dry. Make sure to follow your surgeon's specific instructions for wound care, including when you can shower and how to change dressings. During this time, a good pair of supportive underwear can provide gentle compression and comfort, which really helps.
By week two, you should be feeling much more like your old self. You’ll be moving around more freely, and any sharp pain will likely have faded to a dull ache, if you feel it at all. Now’s the time to slowly reintroduce light activities.
Most people feel ready to drive again after about two weeks, once they’re off strong painkillers and can perform an emergency stop without pain. Getting back to work depends on what you do.
The key is to listen to your body. Don't push it. Gentle walking is your best friend right now; it prevents stiffness and improves blood flow without putting any strain on the repair. Getting your movement patterns right is vital, and some patients find that guided professional support helps them regain strength and confidence. Exploring comprehensive physiotherapy services at The Vesey can be a great step in planning a full return to form.
Once you hit the one-month mark, you’re on the home stretch. Most of the crucial internal healing happens over the first six weeks, as the mesh fully integrates with your body’s tissues. Around this time, your surgeon will likely give you the green light to resume more strenuous exercise.
When you do start again, take it slow and build up the intensity gradually. The single most important rule is to avoid heavy lifting (anything over 10kg) for at least six weeks, or for as long as your surgeon advises. Sticking to this is the best way to prevent the hernia from coming back.
While recovery is usually straightforward, you need to know what to watch out for.
Get in touch with your doctor if you experience:
By following your surgeon's advice and giving your body the time it needs to heal, you can look forward to a successful recovery and a life free from the pain and hassle of a hernia.
Deciding on any kind of surgery means weighing up the good with the bad. An inguinal hernia repair is one of the most common and safest operations performed today, but it’s still important to go in with your eyes open. The aim is to feel confident in your decision, knowing both the significant advantages and the possible complications.
The main benefit is simple: relief. Repairing the hernia gets rid of that nagging ache, pressure, or sharp pain that messes with your day-to-day life. It means you can stand up, walk, cough, or lift something without that all-too-familiar groin discomfort.
But it’s about more than just pain relief. The surgery gives you your freedom back. It’s about returning to the things you enjoy, whether that’s a round of golf, playing with your grandkids, or just getting through a day’s work without wincing. It’s about restoring your quality of life.
One of the most critical reasons for surgery is prevention. Left alone, a hernia can get trapped (incarcerated) or, worse, have its blood supply cut off (strangulated). These are both medical emergencies that demand immediate, more complicated surgery and come with much higher risks.
A planned hernia repair neatly closes the door on these dangerous outcomes. It’s a proactive step that solves the problem before it has a chance to turn into a serious health crisis, giving you genuine long-term peace of mind.
Like any operation, hernia repair isn’t completely without risk, although major complications are thankfully rare. Knowing what they are helps you understand what to watch for during recovery and allows you to have a much better conversation with your surgeon.
Most of the issues people run into are minor and don't last long. These include:
These common side effects are just part of the healing journey. However, there are a few less common but more significant risks to be aware of.
While the overall success rate for inguinal hernia repair is very high, a small percentage of patients may experience longer-term issues. Understanding these possibilities is a key part of the consent process and helps set realistic expectations for recovery.
Rarer complications can include nerve irritation, which might lead to some numbness or persistent pain in the groin area. Chronic groin pain, lasting more than three months after surgery, is an important point to consider, though it only affects a small number of patients. Advances in surgical techniques and a huge focus on carefully protecting the nerves have helped bring this risk right down.
Your surgical team is completely focused on your well-being, and multiple protocols are in place for enhancing surgical safety and reducing risks. Having an open chat with your surgeon is key. They will explain exactly how they plan to minimise these risks for you, based on your health and the specific technique they’ll be using. This ensures you can make a decision that feels right, backed by a clear understanding of the whole picture.
Even after we've gone through the details of an inguinal hernia repair, it’s completely normal to have more questions about what life will look like afterwards. Let's clear up a few of the most common queries we hear from patients so you can feel confident about the road ahead.
This really comes down to what you do for a living. There’s no one-size-fits-all answer, as the physical demands of your job are the biggest factor.
If you have a desk-based or administrative role, you’ll likely bounce back quite quickly. Most people in these jobs are back at work within one to two weeks. However, if your job involves manual labour, heavy lifting, or any kind of serious physical strain, you absolutely must give your body more time to heal. For these physically demanding roles, you should plan for four to six weeks off to ensure the repair is solid.
Your surgeon will give you a personalised recommendation based on your specific procedure and job.
It’s possible, but not common. Modern hernia repair, particularly with the use of surgical mesh, has been a game-changer, dramatically lowering the risk of the hernia returning.
Statistically, the chance of an inguinal hernia recurring after a mesh repair is very low, typically sitting between 1% and 3%. This is a huge improvement on older, non-mesh techniques.
The best thing you can do to prevent a recurrence is to follow your post-operative instructions to the letter. That means sticking to the lifting restrictions and avoiding strenuous activity for that crucial initial six-week healing period. Giving your body the time it needs to heal properly is your best defence.
A scar is a natural part of the healing process after any operation. The type of scar you'll have depends entirely on which surgical technique was used.
Once the wound has fully healed, your surgical team can give you practical tips on scar care, like gentle massage or using silicone strips, to help minimise its appearance.
Yes, absolutely. This is not only normal but also very common and expected after an inguinal hernia repair. You might notice swelling and bruising around the groin, which can sometimes track down into the genital area. This is just your body’s standard response to surgery.
It usually peaks a few days after the operation and then gradually fades over the next one to two weeks. To help manage it in the first 48 hours, gently applying an ice pack (wrapped in a cloth) to the area for 15-20 minutes at a time can make a big difference to both the swelling and any discomfort. Rest assured, it's a temporary and normal part of your recovery.
At The Vesey Private Hospital Ltd, our expert surgical team is dedicated to providing personalised care, from your first consultation right through to your full recovery. If you have more questions or would like to discuss your options for inguinal hernia repair, we're here to help you make an informed decision with confidence. You can find out more about our services at https://www.thevesey.co.uk.

At The Vesey Private Hospital Ltd, our expert surgical team is dedicated to providing personalised care, from your first consultation right through to your full recovery. If you have more questions or would like to discuss your options for inguinal hernia repair, we're here to help you make an informed decision with confidence. You can find out more about our services at https://www.thevesey.co.uk.