.webp)
If you're dealing with chronic knee pain that’s stopping you from doing the things you love, you’ve probably heard about knee replacements. But it's not a one-size-fits-all solution. For some people, a partial knee replacement is a far better, more targeted option.
Think of it like fixing a single pothole in a road instead of repaving the entire street. It’s a less invasive surgery that replaces only the damaged part of your knee with an implant, leaving all the healthy bone, cartilage, and ligaments completely untouched. This approach is designed specifically for people whose arthritis is confined to just one area of the joint.
When osteoarthritis takes hold, it wears away the smooth cartilage that cushions your joints. This is what causes that painful bone-on-bone friction that can turn a simple walk or a flight of stairs into a real challenge.
While many people assume a "knee replacement" means a total overhaul, there are actually different approaches tailored to the exact pattern of damage in your knee. A partial knee replacement, known in the medical world as a unicompartmental knee arthroplasty, is a specialised procedure for when arthritis has only affected one of the knee's three compartments.
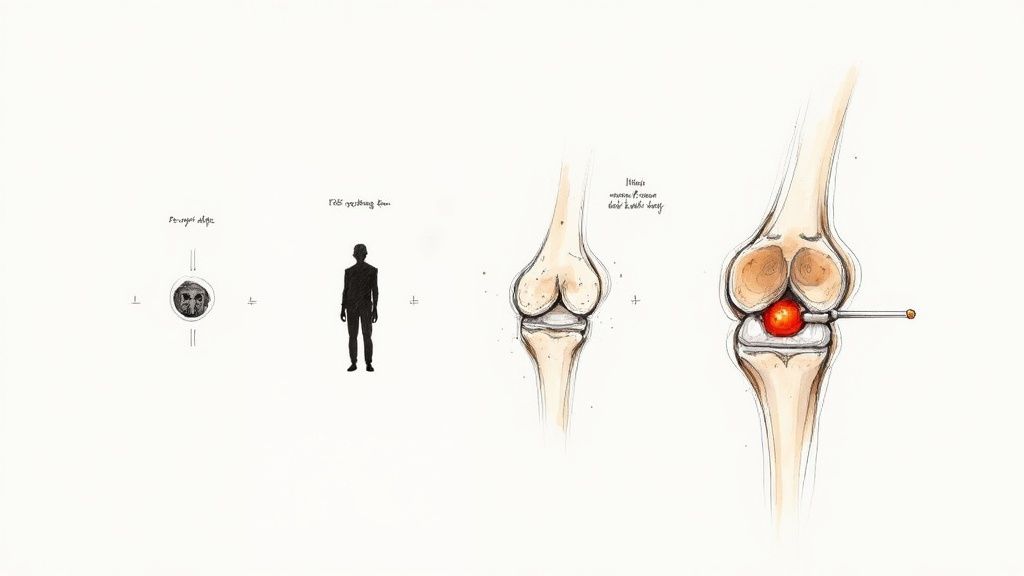
To really get your head around how a partial replacement works, it helps to picture the knee as a structure with three distinct sections, or compartments, where your thighbone (femur) and shinbone (tibia) meet:
If osteoarthritis has only damaged one of these areas—and it's most often the medial compartment—while the other two are still healthy and stable, you could be a perfect candidate for this more focused surgical fix.
A partial knee replacement is fundamentally about preservation. The goal is to correct the specific problem area while leaving as much of your natural, healthy knee anatomy intact as possible. This is the key difference when compared to a total knee replacement.
The distinction between a partial and a total knee replacement (TKR) is a crucial one. During a total knee replacement, the surgeon resurfaces all three compartments. It’s a comprehensive solution, but it’s best suited for widespread arthritis that has affected the entire joint.
A partial knee replacement, on the other hand, is all about precision. The surgeon makes a much smaller incision, removes only the damaged cartilage and bone in the single problem compartment, and then fits a precisely-sized implant in that specific area. The healthy cartilage elsewhere is left alone, and crucial stabilising ligaments like the anterior cruciate ligament (ACL) are preserved.
Surgeons here in the UK are very careful when assessing if a partial knee replacement is the right call. While every person is unique, the ideal candidate usually fits a clear profile. This precise targeting is exactly why understanding your options for joint replacement surgery is so important for getting the best outcome.
Key things we look for include:
This procedure is often a fantastic choice for people who are still active and want to maintain a more natural-feeling knee. By focusing only on the problem area, it offers a path to pain relief while keeping the parts of the joint that are still working perfectly.
So, is a partial knee replacement the right move for you? That decision comes down to a careful evaluation by your surgeon, and it all starts with one crucial factor: the precise location of your arthritis. If the damage is neatly confined to a single area of the knee, this targeted procedure becomes a very real possibility.
Think of your knee joint as having three main compartments where your thighbone (femur) and shinbone (tibia) meet. You have the medial (inner) side, the lateral (outer) side, and the patellofemoral compartment at the front, behind your kneecap. A partial knee replacement is specifically designed for people whose osteoarthritis is isolated to just one of these compartments, while the other two remain healthy and functional.
To get the full picture, your surgeon will combine a hands-on physical examination with imaging, usually X-rays. This detailed assessment is what confirms whether your pain and cartilage damage are truly localised. It’s the first and most important green light.
Beyond the location of the arthritis, a few other things need to line up. An ideal candidate for a partial knee replacement generally has:
This procedure is fairly common in the UK, though its use can vary between NHS trusts. Looking at the data from the National Joint Registry, partial knee replacements make up about 7% to 8% of all knee procedures each year. It's also interesting to note that male patients account for around 55% of those undergoing this specific surgery.
Just as important as knowing who is a good candidate is understanding who isn’t. There are certain situations, known as contraindications, where this procedure simply isn't the best option.
A surgeon will almost always advise against a partial knee replacement if you have conditions that could undermine the result.
The success of a partial knee replacement hinges on the health of the rest of your knee. If other parts of the joint are weak or diseased, resurfacing only one compartment won't provide a stable, long-term solution.
Common reasons to rule it out include:
This decision-making process helps your surgeon determine if your knee pain is suitable for this highly specific surgery.
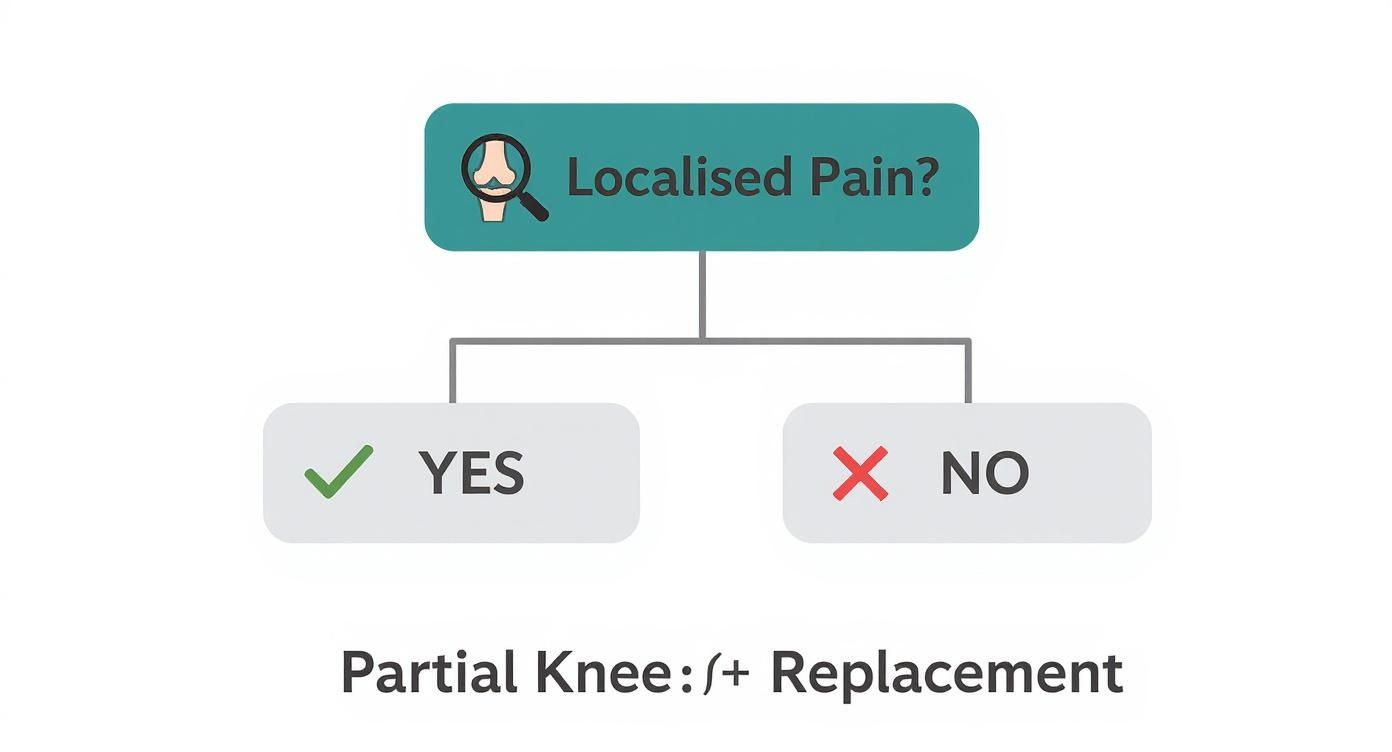
As you can see, localised pain is the first and most critical checkpoint on the path to even considering a partial knee replacement. From there, the other factors help build a complete picture of your suitability.
Knowing what to expect on the day of your operation can make a huge difference, helping you feel prepared and less anxious. A partial knee replacement is a meticulously planned procedure, and your surgical team follows a precise set of steps designed to give you the best possible result. Let's walk through what happens, from the moment you arrive at the hospital to the final stitch.
Your journey actually begins long before the day itself with thorough pre-operative planning. Using detailed imaging like X-rays and sometimes MRI scans, your surgeon creates a precise blueprint for the procedure. This allows them to map out your unique knee anatomy and select the perfectly sized implant ahead of time.
On the day of surgery, you’ll meet your anaesthetist to discuss the best way to keep you comfortable. For a partial knee replacement in the UK, a few options are common, and the final decision is usually made together.
Your anaesthetist will recommend the safest and most effective choice based on your health and personal preference. Once that’s sorted, you’ll be taken to the operating theatre.
The main event—the operation itself—is a fantastic example of a minimally invasive technique. The whole goal is to fix the problem area with as little disruption to the healthy parts of your knee as possible.
The entire partial knee replacement procedure is remarkably efficient. From the first cut to the last stitch, it’s usually all done within 60 to 90 minutes.
In recent years, surgical precision has taken another leap forward with technology. Many UK surgeons now use robotic-assisted systems to perform partial knee replacements. It’s important to understand that the robot doesn’t perform the surgery; it acts as an incredibly precise guide for the surgeon.
Using data specific to your knee's anatomy, the robotic arm helps the surgeon prepare the bone and place the implant with an exceptional degree of accuracy. This level of precision can lead to better implant alignment and function, which may improve long-term outcomes. If you're keen to know more, you can delve into the details of these advanced knee replacement procedures and see how they benefit patients.
By the time you wake up in the recovery room, your surgical journey is complete, and the next chapter—your rehabilitation—can begin.
Making a smart decision about surgery means looking at the full picture—both the upsides and the potential downsides. A partial knee replacement is less invasive than a full one, and that brings some powerful advantages for the right person. Of course, like any operation, it isn't without its risks.
The key is to understand this balance. When you can weigh the pros and cons clearly, you can have a much better conversation with your surgeon and decide if this is truly the right path for your health and your lifestyle.
For a well-suited candidate, the benefits of a partial knee replacement often lead to a much smoother surgical experience and a better long-term result. Because the procedure keeps so much of your natural knee intact, the positive effects are often felt almost immediately.
The main benefits usually include:
The real magic of a partial knee replacement is its principle of preservation. By only targeting the damaged area, it respects the healthy, functioning parts of your joint, which often leads to a more natural and functional feeling in the long run.
This patient-centred approach is becoming more popular across the UK. While total knee replacements are still more common, partial knee replacements are a fast-growing option, especially for younger, more active individuals. In fact, the UK knee implants market is set to grow at a compound annual rate of about 3.2% through 2030, partly driven by this shift. You can find more details in this analysis of UK market trends and forecasts.
While a partial knee replacement is a very successful procedure for most, it's vital to be aware of the potential risks. These can be broken down into general surgical risks and a few that are more specific to this particular operation.
Your surgical team takes every possible precaution to minimise these risks, but a well-informed patient is always the safest. Knowing what to look out for helps you spot any warning signs and play an active role in your own care.
General risks for any surgery include:
Procedure-specific risks you should consider are:
Going over these possibilities with your surgeon will help you feel fully prepared and confident about the path you choose.

The success of your partial knee replacement doesn't end when you leave the operating theatre. In fact, a huge part of your long-term result hinges on what you do next. Your commitment to a structured recovery plan is every bit as important as the surgery itself.
Think of the weeks after your operation as building the foundations for your new knee. It's a partnership between you and your physiotherapy team, and your active participation is the key ingredient for a brilliant outcome. Let’s walk through the milestones ahead.
Your recovery starts almost immediately—often on the very same day as your surgery. A physiotherapist will help you get out of bed and take your first few steps, using a frame or crutches for support. Early movement like this is crucial for preventing stiffness and complications like blood clots.
In these first couple of days, the focus is on simple but vital goals. You’ll learn how to get in and out of bed safely, walk short distances, and even manage stairs. The team will also introduce gentle exercises to wake up the muscles around your knee and get the blood flowing.
One of the big advantages of a partial knee replacement is the shorter hospital stay. Because the surgery is less invasive, patients are on their feet much quicker. In England, the median length of stay has dropped to just 1.91 days, a massive improvement and significantly shorter than the average for a total knee replacement.
Once you’re home, the real work begins. For the next six weeks, your focus will be on managing any swelling, keeping pain under control, and sticking diligently to your physiotherapy exercises. This is where you build the strength and flexibility you’ll need for everyday life.
Your physiotherapy sessions will become more progressive, with exercises designed to achieve specific goals:
Consistency is your best friend during this phase. Doing your exercises multiple times a day, just as you're shown, is far more effective than one long, occasional session. Little and often is the mantra.
By the end of six weeks, most people can walk comfortably without crutches and have seen a huge improvement in their knee’s flexibility. This is often when you can start thinking about driving again, as long as you can perform an emergency stop without pain.
This next phase is all about building on that solid foundation and gradually reintroducing your normal activities. Your physiotherapy will start to look more like real-world movements, helping you get back to your routine. Your strength and endurance will keep improving, and you’ll notice a big drop in pain and stiffness.
Key milestones during this period often include:
A key part of rehab is keeping track of your progress, including understanding how to measure range of motion accurately. Seeing these improvements helps both you and your physiotherapist know you’re on the right track. For more detail on what to expect, our guide on comprehensive physiotherapy services can offer further insight.
From three months onwards, you’ll continue to see gradual improvements in strength and function for up to a year. The deep surgical ache will fade, and your confidence in your new knee will really start to grow. This is often when you can return to more demanding hobbies like doubles tennis, golf, or hiking.
The most important thing is to listen to your body. Your new partial knee is durable, but it’s wise to favour low-impact activities to ensure it lasts for the long haul. By staying active and maintaining a healthy weight, you give your new joint the best possible chance to provide decades of pain-free movement.
Even after getting your head around the procedure and recovery, it's completely normal to have a few more specific questions. What does life really look like after a partial knee replacement? Here are the answers to some of the most common queries we hear from patients, designed to give you clarity and confidence.
This is usually the first question people ask, and for good reason. You want a solution that’s going to go the distance. The great news is that modern partial knee implants have an excellent track record.
Extensive studies and registry data show that more than 90% of partial knee replacements are still working well 10 to 15 years after the operation. Many people get two decades or more of pain-free activity before needing any further help.
Of course, a few things can influence how long your new joint lasts:
While they might have a slightly higher revision rate over a very long period compared to a total knee replacement, the trade-off is often a much faster recovery and a knee that feels more natural for years.
One of the main goals here is to get you back to an active, enjoyable lifestyle. A partial knee replacement is designed to feel more natural, which opens the door to a much greater range of motion and makes many activities possible again.
Once you’re fully recovered, your surgeon will encourage you to embrace a whole range of low-impact exercises. These are fantastic not just for your new knee, but for your overall health too.
The aim is to stay active while being smart about protecting your new joint. Think of it as choosing activities that strengthen your body without placing excessive force on the implant.
Your new "approved" activity list will likely include:
On the flip side, activities that involve high impact—like running, jumping, or contact sports such as football—are generally off the cards. The repetitive jarring can wear down the plastic component and shorten the implant's lifespan. The focus is on finding a sustainable, active routine you can enjoy for years.
While a partial knee replacement is designed to be a long-term fix, it's true that some people may need another operation down the line. The most common reason for this "revision" surgery is that arthritis has started to progress in the other parts of the knee—the ones that were initially healthy.
Think back to the three compartments of the knee. Your surgery fixed the one damaged area, but the other two were left in their natural state. If arthritis develops in one of those compartments years later, you might start to feel pain again.
The good news is that this is a very straightforward problem to solve. Converting a partial knee replacement to a total one is a standard and highly successful procedure. Your surgeon can simply remove the partial implant and perform a full replacement, resurfacing all three compartments. It’s a well-trodden path with excellent outcomes. For anyone concerned about financing such procedures, our overview of the typical knee replacement cost in the UK can provide some valuable context.
Ultimately, having a partial knee replacement first gives many people years of fantastic function with a more natural-feeling knee. And if things do change in the future, you still have a highly effective solution in reserve.
At The Vesey Private Hospital, our expert orthopaedic consultants are here to answer all your questions and help you decide on the best treatment path for your knee pain. To explore your options and book a consultation, please visit us at https://www.thevesey.co.uk.

