.webp)
It’s easy to mistake silent reflux for a common cold or a stubborn allergy. It often shows up as a persistent cough, that annoying need to constantly clear your throat, or a frustrating feeling like there’s a lump stuck in your throat.
This sneaky condition, known properly as Laryngopharyngeal Reflux (LPR), causes real irritation but cleverly avoids the classic heartburn that most people associate with acid reflux.
Think of silent reflux as a "smokeless fire." Unlike the obvious alarm bells of GORD (Gastro-oesophageal Reflux Disease), LPR doesn't always set off that fiery sensation in your chest. Instead, tiny droplets of stomach acid and digestive enzymes like pepsin travel all the way up your oesophagus and settle in the delicate tissues of your throat and voice box.
These areas simply aren't built to handle stomach contents. The result? A confusing mix of symptoms that are all too easy to misdiagnose:
This condition is surprisingly common. In fact, some studies suggest that around 34.4% of the UK population may experience LPR-related issues, with many having no idea what’s really causing their discomfort.
It’s this "silent" nature that makes spotting the symptoms the first and most important step toward getting things sorted.
It’s a fair question. When you’re dealing with a nagging cough or a voice that keeps disappearing, your symptoms feel anything but silent. The name actually comes from what’s missing when we compare Laryngopharyngeal Reflux (LPR) to its more famous cousin, Gastro-oesophageal Reflux Disease (GORD).
GORD is the one everyone knows about. It’s the “noisy” reflux that usually announces itself with that classic, unmistakable burning feeling in your chest – heartburn.
Silent reflux, on the other hand, often skips the chest pain entirely. The issue isn't just stomach acid, but also a digestive enzyme called pepsin. While perfectly safe in your stomach, pepsin becomes a serious irritant when it travels up into the delicate tissues of your throat and voice box.
Here’s a good way to picture the difference. Think of GORD as a pot of water boiling over on the hob. It's hot, dramatic, and you feel the burn in your chest right away.
LPR is more like a fine, cool mist rising from that same pot.
This mist travels much higher up, bypassing the oesophagus and settling into your airways. It doesn’t "burn" in the same way, but its constant, quiet presence irritates sensitive areas that were never designed to handle it, causing a slow build-up of inflammation.
This stealthy mechanism is exactly why the symptoms are centred in your throat, not your chest. That irritation from pepsin is what triggers the chronic cough, hoarseness, and that frustrating feeling of having a lump in your throat.
Recognising this subtle difference is the key to understanding why the condition can be so tricky to pin down. A specialist can get a direct look at these areas for tell-tale signs of irritation. Diagnostic procedures like a laryngoscopy and pharyngoscopy are often used to confirm what’s going on. Ultimately, it’s the absence of classic heartburn that makes the reflux "silent" to traditional assumptions.
The signs of silent reflux in adults can be frustratingly subtle, often masquerading as common, everyday problems. That raspy, hoarse voice you wake up with? You might blame it on a bad night's sleep, but it's a classic sign of LPR.
Another tell-tale symptom is that annoying feeling of a lump stuck in your throat, a sensation medically known as globus sensation. It’s not actually a lump, but it feels just like one.
These feelings pop up because the delicate tissues in your voice box (larynx) and throat (pharynx) aren't built to handle stomach enzymes like pepsin. Unlike the tougher oesophagus, even tiny amounts of exposure can cause significant irritation, kicking off a cycle of confusing symptoms.
Many people finally connect the dots when they notice their symptoms get worse after eating or when they lie down at night.
The most common signs of silent reflux to watch out for include:
This infographic breaks down how silent reflux (LPR) creates that "mist-like" effect in the upper airways, compared to the more familiar heartburn of classic GORD.
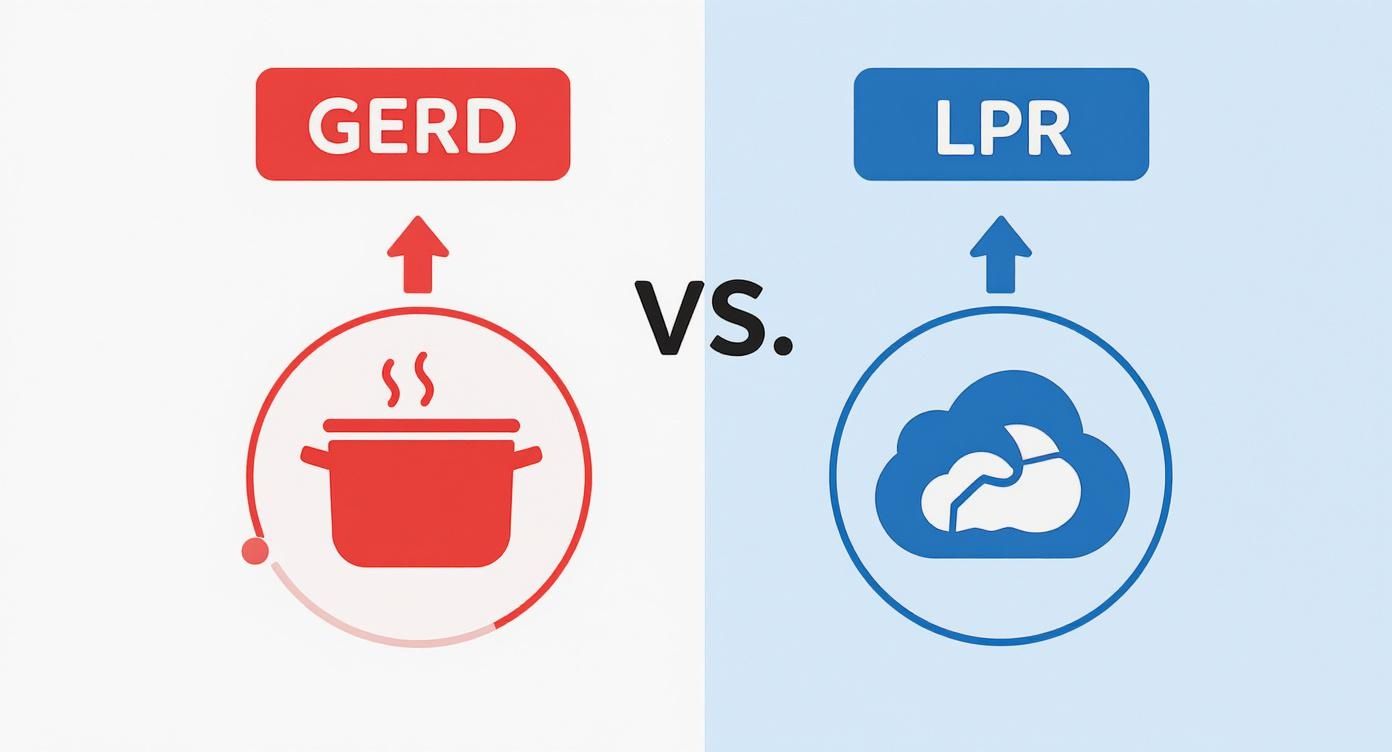
As the visual shows, LPR primarily affects your throat and voice box, while GORD is focused on the lower oesophagus. This is why the symptoms feel so different.
Because these signs overlap so much with other conditions, it's incredibly easy to misdiagnose what's going on. In fact, many are similar to what you'd find in classic reflux; you can explore the full range of symptoms of acid reflux in our other guide. Learning to spot the difference is key to getting the right help.
It's a common dilemma: is that persistent cough and sore throat down to LPR, or is it just a lingering cold or hay fever? The symptoms can be incredibly similar, but there are a few clues that can help you tell them apart.
This table highlights the key differences:
SymptomSilent Reflux (LPR)Cold/AllergiesCoughDry, persistent, often worse at night or after meals.Can be wet or dry; often comes with other symptoms like sneezing or a runny nose.Sore Throat/HoarsenessChronic, often worst in the morning. Feels like a lump.Usually acute and improves within a week. May feel scratchy.Post-Nasal DripConstant feeling of thick mucus, leading to throat clearing.Typically accompanied by sneezing, itchy eyes, or a blocked/runny nose.TriggersTriggered by food (spicy, fatty, acidic), lying down, or large meals.Triggered by viruses (cold) or allergens like pollen, dust, or pet dander (allergies).Other SymptomsRarely includes fever, body aches, or itchy eyes.Often includes sneezing, runny nose, watery eyes, fever (cold), or body aches.
While this table can point you in the right direction, remember that it's not a substitute for a proper diagnosis. If your symptoms are persistent and you're just not sure what's causing them, it's always best to have a chat with a doctor. They can help you get to the bottom of it.
Spotting silent reflux in babies and children can be incredibly stressful for parents, mainly because the symptoms look so different from what we see in adults. While a little bit of ‘spitting up’ is perfectly normal for most infants, persistent and problematic reflux is another matter entirely.
The classic signs in babies often don't involve obvious vomiting at all. Instead, you might notice your little one is unusually irritable during or after a feed, struggles with poor weight gain, or even has breathing difficulties like a rattly chest or wheezing. These are subtle but significant clues. For a wider look at the topic, this guide on acid reflux in babies is a helpful resource.
As children get older, the silent reflux symptoms can change yet again, sometimes becoming even more disguised. What you might put down to a constant case of the sniffles could actually be a sign of underlying reflux.
Keep an eye out for these less obvious indicators:
Because these symptoms mimic so many other common childhood illnesses, it's easy for the root cause to be missed. Realising that recurring issues like constant ear trouble could be linked to reflux is the first step towards getting the right support.
Knowing what’s normal and what might need a closer look is crucial. For parents navigating these challenges, finding resources on diet is a great next step. You can find more practical guidance in our article covering dietary advice for children.
If you’re ever concerned about any of these signs, speaking with a paediatrician is always the best course of action.
Getting the right diagnosis for silent reflux is often a journey of persistence. Why? Because its symptoms are so easily mistaken for other conditions. Many people first see their GP for a nagging cough or a permanently hoarse voice, only to find that the usual treatments for allergies or chest infections just don’t work.
This is where the real diagnostic path begins. If your GP suspects something more is going on, specifically Laryngopharyngeal Reflux (LPR), they may refer you for a specialist opinion. An ear, nose, and throat (ENT) assessment is really the gold standard for getting to the bottom of throat-related silent reflux symptoms.
An ENT specialist has a few specific tools up their sleeve to uncover the subtle clues of LPR. The process usually kicks off with a detailed chat about what you've been experiencing, often using a questionnaire to guide the conversation.
One of the most common tools is the Reflux Symptom Index (RSI). It’s a simple scoring system where you rate the severity of issues like hoarseness, constant throat clearing, and that annoying lump-in-the-throat feeling. A high score is a strong pointer towards LPR.
The next step is often to have a direct look at the area in question with a procedure called a laryngoscopy. This involves passing a tiny, flexible camera through your nose and down into your throat to get a clear view of your voice box. The specialist is looking for tell-tale signs of irritation, redness, and swelling caused by acid and enzymes.
This visual evidence is crucial. It confirms that the symptoms you’re feeling have a physical cause, even if you never experience classic heartburn.
However, LPR can be a tricky thing to pin down. Research shows that it can exist even without obvious symptoms, and what a specialist sees during a laryngoscopy doesn't always match how severe a person feels their issues are. This variability is exactly why a thorough evaluation by an expert is so vital for getting an accurate diagnosis and, more importantly, a treatment plan that actually works.
As we get older, our bodies naturally change, and the muscles controlling the valve between our stomach and oesophagus are no exception. Think of these oesophageal sphincters as gatekeepers, designed to keep stomach acid and food exactly where they belong. With time, they can lose some of their tightness and strength, making it that much easier for reflux to sneak past.
This isn't just a theory; we see it in clinical practice. Studies in UK ENT clinics found that over 25% of patients with upper gastrointestinal symptoms showed clear signs of LPR. The research also pinpointed the highest concentrations of pepsin—a key enzyme that causes irritation in silent reflux—in patients over the age of 80. You can read more about the findings linking age to reflux severity.
But age is only one piece of the puzzle. Your daily habits and choices play a massive role in either taming or triggering your silent reflux symptoms.
Lifestyle factors can directly influence how often those gatekeeper muscles relax and how much pressure builds up in your stomach. Getting to grips with this connection is the first real step toward feeling better.
Some of the most common lifestyle contributors include:
When looking at how lifestyle affects reflux, exploring natural ways to support digestive comfort and acid reflux is a great place to start. By figuring out your personal triggers, you can begin making changes that truly count.
Living with silent reflux can bring up a lot of questions. Getting clear, practical answers is the first step towards managing your symptoms and feeling more in control of your health.
Let's tackle some of the most common queries we hear.
Yes, absolutely. In fact, this is the defining feature of Laryngopharyngeal Reflux (LPR).
Stomach contents, including acid and enzymes like pepsin, travel all the way up to the throat and voice box. But unlike GORD, they often don't cause that classic fiery chest pain. This is precisely why the main silent reflux symptoms are things like a hoarse voice, a persistent cough, or constant throat clearing, rather than digestive discomfort.
Diet and lifestyle adjustments are the bedrock of LPR management. The first step is to identify and avoid common trigger foods—things like caffeine, spicy meals, alcohol, and fatty foods are frequent culprits.
Beyond diet, these strategies are highly effective:
You should book an appointment with your GP if your symptoms have been hanging around for more than a few weeks, especially if they're starting to affect your quality of life.
It's particularly important to seek medical advice if you notice any "red flag" symptoms. This includes unexplained weight loss, significant pain when you swallow, or a change in your voice that lasts longer than a fortnight.
A doctor can properly diagnose the issue, rule out other causes, and guide you on the best next steps.
If persistent throat symptoms are impacting your daily life, don't just wait for them to go away. The specialists at The Vesey can provide a thorough assessment and create a personalised treatment plan to help you find lasting relief. Visit https://www.thevesey.co.uk to book your consultation today.

If persistent throat symptoms are impacting your daily life, don't just wait for them to go away. The specialists at The Vesey can provide a thorough assessment and create a personalised treatment plan to help you find lasting relief. Visit https://www.thevesey.co.uk to book your consultation today.