.webp)
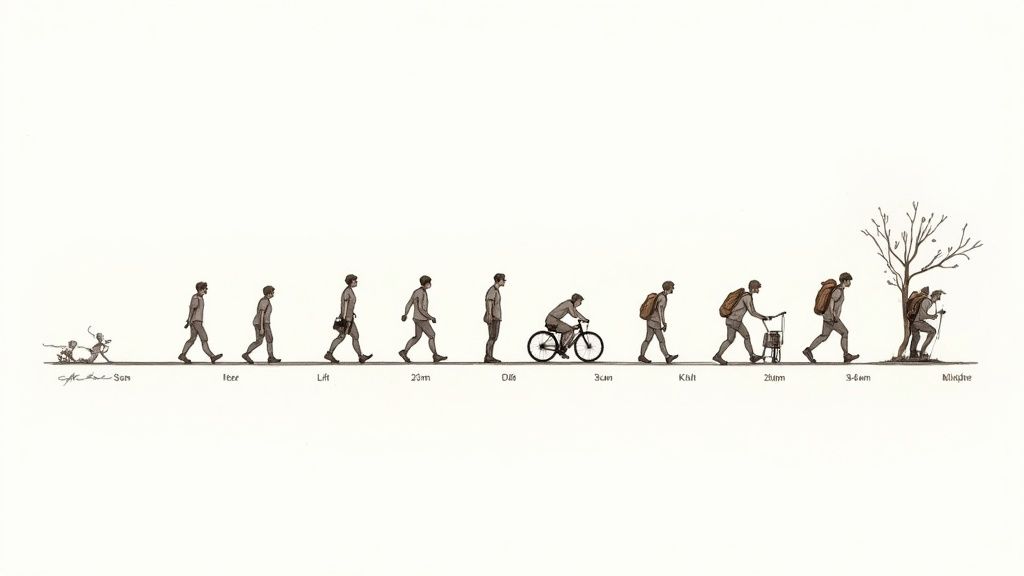
A full recovery from a total knee replacement can take up to a year, but you'll hit significant milestones much sooner than that. Most people are back to light activities within 3 to 6 months, with the most intense part of the recovery happening in the first six weeks after surgery.
Having a total knee replacement is a huge step towards getting your pain-free life back, but it’s just as important to understand what comes next. The best way to think about your recovery is as a series of stages, each with its own goals and challenges. Think of it as a roadmap guiding you from those first few days after surgery all the way to moving with full confidence again.
This journey isn't a sprint; it’s a marathon paced with steady, consistent effort. The first few weeks are all about the fundamentals: getting pain under control, reducing swelling, and starting gentle physiotherapy to get your knee’s range of motion back. As you get stronger, the focus will shift to building strength and endurance, letting you gradually reclaim your independence.
Everyone’s experience is slightly different, but the path to recovery generally follows a predictable pattern. The specific technology and techniques used in your operation can also influence how quickly you progress. You can learn more about the different options in our guide to advanced knee replacement procedures.
The trick is to set realistic goals for each phase. Success is built on being patient and sticking to your rehabilitation plan.
The table below gives you a quick summary of what to expect at the critical points along your total knee replacement recovery timeline.
TimeframeKey FocusMobility GoalsPain & SwellingFirst WeekPain control, wound care, early mobilisationWalking short distances with a frame or crutchesHighest levels, managed with medication and elevationFirst MonthRegaining range of motion, light exercisesProgressing to a single crutch or caneNoticeably decreasing but still present3-6 MonthsBuilding strength and enduranceWalking without assistance, low-impact activitiesMinimal, often occurring only after activityOne YearFull functional recovery and strengthReturning to most desired recreational activitiesLargely resolved, with occasional minor stiffness
This visual timeline gives a great overview of the progression, from those early days in the hospital to regaining an active lifestyle over the course of a year.
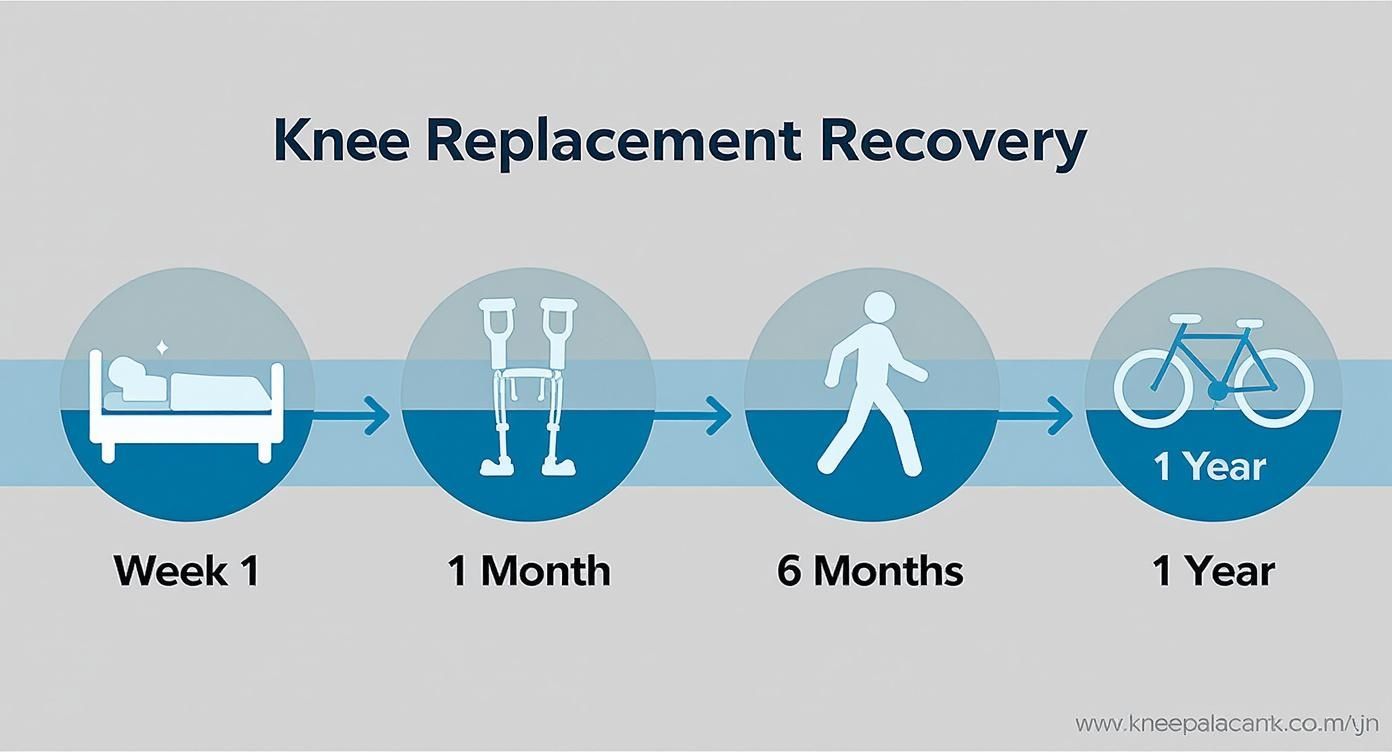
As you can see from the infographic, the journey is all about a gradual shift. You'll move from needing walking aids to moving independently, and finally, to getting back to the more vigorous activities you love.
The moment you wake up from surgery, your recovery timeline has officially begun. Think of this initial hospital stay as laying the foundation for a great outcome. Your body has just been through a major event, and these first 48 hours are all about managing the immediate after-effects and kickstarting the healing process with experts by your side.
The biggest focus, right off the bat, is your comfort and safety. Pain is completely normal at this early stage, but your healthcare team will have a solid plan to keep it under control. This usually involves a mix of medications. Your anaesthetist may have used specific techniques, which you can learn more about in our guide on nerve block procedures for pain relief.
Getting pain under control isn’t just about feeling better—it's what makes the next critical step possible: getting you moving. Your clinical team will want to see you moving safely, often within the first 24 hours.
A physiotherapist will come to see you and guide you through those first few movements. It’ll start small, probably just sitting up in bed, then standing, and maybe taking a few steps with a walking frame or crutches. These small wins are a huge deal for a few reasons:
At the same time, your nurses will be keeping a close eye on your surgical wound, making sure the dressing is clean and secure to head off any risk of infection. They'll also show you how to look after the incision, a skill you’ll need once you get home.
"The goal of early mobilisation is not to push you to your limits, but to gently reintroduce movement. It is the single most important activity in the first few days to set the stage for a smoother, faster recovery."
During these first couple of days, you're in the hands of a whole team. Nurses will be managing your pain relief and daily needs, while the physios design and oversee your exercise programme. They all work together, making sure you hit key milestones before it's safe for you to be discharged.
How long you stay in hospital can vary. An analysis of NHS statistics in England found that the average hospital stay is just over four days. Around 20% of patients stay a bit longer, and very few—less than 1%—go home on the same day as their surgery. You can read more about these hospital stay findings and what they mean for patients.
Once you’re back from the hospital, your home becomes the centre of your recovery. This initial six-week period is the most intensive phase of your total knee replacement journey. It’s all about getting into a solid routine that will set you up for long-term mobility and a successful outcome.
Think of this stage as getting to know your new knee. The focus is threefold: keeping pain and swelling under control, looking after your surgical wound, and sticking to your prescribed exercises. You'll quickly learn its limits, figure out how to manage discomfort, and start building its strength, day by day.
Pain and swelling are completely normal after surgery, and you’ll notice them most in these first few weeks. Managing them well is crucial because it makes it easier to engage with your physiotherapy. Your surgeon will have prescribed pain medication—it's important to take it as directed to stay on top of the discomfort, not just react to it.
Beyond medication, simple actions can make a huge difference. Regular icing is one of your best tools against inflammation; aim for about 15-20 minutes several times a day. Elevating your leg is also key. You can learn more about the health benefits of elevating your legs to help dial down the discomfort and give your body the best chance to heal.
Physiotherapy is the engine of your recovery. During these first six weeks, the exercises aren't about becoming an athlete; they're designed to achieve two fundamental goals:
Consistency is far more important than intensity right now. Doing short, frequent exercise sessions throughout the day is much better than one long, exhausting workout. This steady, gentle effort prevents scar tissue from building up and gradually improves how your knee functions. For more insight into what this involves, you can explore our information on comprehensive physiotherapy services.
Your dedication to your home exercise programme during this foundational period directly influences the quality and speed of your recovery. Each small repetition is a step towards regaining your independence.
Your mobility will improve week by week. You'll likely start with a walker or two crutches to move around safely without putting too much weight on your new knee. As your balance and strength improve, your physio will guide you on when it’s safe to transition to a single crutch or a cane.
This is a time for gradually getting back to normal life. Simple things like getting dressed, making a cup of tea, or walking to the letterbox become real milestones. It's a time for patience and celebrating the small wins. By the end of this six-week phase, most people feel a significant drop in pain and a clear improvement in their walking and ability to manage daily tasks, which perfectly sets the stage for the next phase of recovery.

This period is often the most rewarding phase of the whole recovery journey. After the intense focus of the first six weeks, you’ll start to notice a real shift. The constant ache begins to subside, your confidence builds, and you finally begin to feel more like your old self again.
This is where all that foundational work really starts to pay off. Think of it like building a house: the first six weeks were about laying the foundation and putting up the frame. Now, you get to install the windows and doors, turning it back into a space you can actually live in. It’s a time of huge progress.
Your physio sessions will start to look a bit different now. The early focus on just getting the knee bending gives way to more dynamic exercises designed to build proper strength and sharpen your balance. Your physiotherapist will introduce new challenges to keep things moving forward.
These advanced exercises are vital for getting your knee ready for the demands of daily life. The goal is to build up the endurance in the muscles that support the joint, letting you walk further, stand for longer, and move with much greater stability. You can explore how different rehabilitation programs for recovery are structured to achieve this.
Key physio goals during this time usually include:
This is often the point where you can get back behind the wheel and return to work, especially if your job is desk-based. Always get the green light from your consultant before driving, as you must be able to perform an emergency stop without a second thought.
The UK recovery timeline for a total knee replacement generally sees most patients achieve significant functional improvement by 12 weeks post-surgery. This progress allows for a confident return to many normal activities.
Many people are also cleared to restart low-impact recreational activities, which is a massive milestone for both physical and mental well-being. Swimming is fantastic because the water supports your body weight, taking the stress off your new joint while providing gentle resistance. A stationary bike is another great, safe way to rebuild strength.
By the 12-week mark, it’s typical to have a lot less pain and much better mobility. This progress is a direct result of sticking with your physiotherapy and carefully reintroducing activity, step by step.
Once you sail past the three-month mark, your total knee replacement recovery enters a new, more empowering phase. The intense, day-by-day focus on pain management and basic movements starts to take a backseat. Now, it’s all about the longer-term goal: building serious strength, endurance, and unshakable confidence in your new joint.
This period, stretching from three months to a full year, is where you really start to see the payoff from all your hard work. Think of the first twelve weeks as learning how to handle a new car—now, you're ready to get it out on the open road. The focus shifts from just getting around the house to actively getting back to the activities you love.
This is the stage where your consultant will likely give you the green light to return to more demanding recreational pastimes. While high-impact sports like running or singles tennis are permanently off the table to protect the implant, a whole new world of activity is ready to open up.
Your physiotherapist becomes your co-pilot here, preparing your body for the specific demands of your chosen hobbies. If you're a keen golfer, they’ll fine-tune your rotational strength and stability for a smooth swing. For hikers, the sessions will centre on building endurance and learning to navigate uneven ground safely.
Getting back in the game requires targeted preparation. For anyone aiming to return to a specific sport, it’s worth exploring the massive benefits of specialised sports physiotherapy services.
Common activities reintroduced during this period include:
Even as you feel stronger and more capable, it’s completely normal to experience some residual symptoms for up to a year. You might notice mild, on-and-off swelling or a touch of stiffness, especially after a long day on your feet or an unusually active session. This is just a sign of your body's final healing stages as it fully adapts to the new joint.
Don’t be discouraged by occasional stiffness or swelling. This is a common experience as your body continues to heal and strengthen for up to a year post-surgery. Consistency with gentle exercise and listening to your body are your best tools.
Managing these lingering symptoms is all about applying the same principles you learned early on. An ice pack after strenuous activity can help reduce any minor swelling, and gentle stretching is perfect for easing stiffness.
The key is to find that sweet spot between pushing your limits to build strength and allowing your body enough time for rest and recovery. This long-term commitment to exercise and maintaining a healthy weight is the single best way to protect your new joint, ensuring it gives you a lasting ticket to a vibrant, active life.
While timelines give you a useful map, your own total knee replacement recovery will have its own unique terrain. Think of the standard schedule as a satnav’s suggested route; your actual trip might involve a few detours based on traffic, weather, and simply how you’re feeling behind the wheel.
Several things influence how quickly you progress. Your fitness level before the operation, your age, and your general health all play a massive part in your body's ability to heal and rebuild. Understanding this from the start helps you set realistic goals and approach your recovery with a positive, informed mindset.
Your recovery speed isn't just about the surgery itself; it’s also about the condition you were in beforehand. For example, a long wait for your operation can take its toll. In England, the median NHS waiting time for knee replacements shot up from 91 days before the pandemic to around 142 days in recent years.
This extended period of pain and limited movement often leads to muscle weakness, which can naturally lengthen the rehabilitation process. You can dig into more data on how waiting times in England have changed.
Other key factors that can influence your recovery include:
It's completely normal to hit a few bumps in the road. Progress is rarely a straight line; some days will feel fantastic, while on others, you might feel a bit stuck. Knowing about these common hurdles can help you navigate them without losing steam.
One of the biggest challenges is disturbed sleep, often caused by discomfort or just struggling to find a comfortable position. Another is managing your expectations around pain. While your new knee will get rid of that deep arthritis ache, the post-surgical recovery brings its own discomfort that gradually fades.
Later on, you might run into muscle tightness or some lingering soreness around the knee. Techniques like foam rolling for knee pain relief can be a great way to help ease these kinds of issues.
"Your recovery timeline is a personal journey, not a competition. Fluctuations in pain, energy, and progress are normal. The goal is steady improvement over time, not perfection every day."
By anticipating these potential challenges, you can prepare strategies to manage them. Staying in close contact with your physio team, celebrating the small wins, and being patient with your body are the keys to a brilliant long-term outcome.
Even with a perfect timeline laid out, you’re bound to have questions as you go. It’s only natural. To help you feel more confident in your journey, here are some straightforward answers to the questions we hear most often from patients recovering from a total knee replacement.
That first wave of significant post-op pain usually eases off within a few weeks, and your prescribed medication will help keep you comfortable. However, it’s completely normal for some mild to moderate swelling and discomfort to stick around for three to six months.
You might even notice a bit of minor swelling up to a year after your operation, especially after you’ve been on your feet all day or pushed yourself a little harder. This is all part of the final stages of healing.
Your best bet for managing these lingering symptoms is to stick to the basics. Consistently using ice packs after activity, elevating your leg when you rest, and listening to your physiotherapist’s advice will make all the difference.
This really comes down to what you do for a living. The physical demands of your job will dictate your return-to-work date.
It’s crucial to have a proper chat with your surgeon about your specific job duties. They’ll give you a personalised and safe recommendation based on your role and your recovery progress.
To protect your new joint and make sure it lasts for years to come, you’ll need to permanently avoid high-impact activities. These movements put too much stress on the implant, which can cause it to wear out prematurely.
Activities to steer clear of include:
Instead, the goal is to embrace low-impact activities. Things like walking, swimming, cycling, and golf are fantastic for maintaining your strength and cardiovascular health without putting your new knee at risk.
Yes, it almost certainly will. Modern knee implants are made from metal alloys that security scanners are designed to pick up.
It's a good idea to give the security staff a heads-up before you walk through the scanner. Some people carry a medical card from their surgeon, but it isn't always a requirement. The main thing is to allow yourself a little extra time to get through airport security without any stress.
At The Vesey Private Hospital, our expert orthopaedic team is here to guide you through every stage of your recovery. If you have more questions or want to discuss your options, we provide rapid access to personalised care. Learn more about our services at The Vesey.

At The Vesey Private Hospital, our expert orthopaedic team is here to guide you through every stage of your recovery. If you have more questions or want to discuss your options, we provide rapid access to personalised care. Learn more about our services at The Vesey.