.webp)
In the UK, the NHS runs a national breast cancer screening programme that's pretty straightforward. The current advice is for women aged 50 to 70 to have a mammogram every three years. The whole point is to catch cancer at its earliest, most treatable stage—a proactive approach that has become a cornerstone of public health, saving thousands of lives each year.

Trying to make sense of healthcare advice can sometimes feel like you’ve been given a map with no compass. Thankfully, the UK’s breast cancer screening guidelines are designed to be a clear, direct route to staying on top of your health. At the heart of it all is the NHS Breast Screening Programme (NHSBSP), a system with one simple goal: find breast cancers early.
Think of it like a routine MOT for your car. It’s a scheduled check-up designed to spot potential issues before they turn into serious problems. This kind of early detection dramatically improves the chances of successful treatment and, ultimately, saves lives.
The programme is all about prevention and catching things before they escalate. By inviting women for regular screenings, the NHS can identify cancers that are far too small to see or feel. This is a game-changer because smaller, early-stage cancers are often less complicated to treat and come with much better long-term outcomes.
The programme works through a few key components:
The NHSBSP is one of the UK’s most important public health initiatives. Its structured approach ensures millions of women have access to life-saving technology, reinforcing the simple truth that early detection is our most powerful tool against breast cancer.
The NHSBSP wasn't just a good idea; it was established back in 1988 based on solid evidence showing that regular mammograms reduce deaths from breast cancer. The results speak for themselves. The programme screens around 1.3 million women every year, diagnosing about 10,000 breast cancers annually through this process alone.
Research has repeatedly confirmed its impact, estimating that it saves approximately 1,400 lives in England every year. To put it another way, for every 400 women screened regularly over a decade, one life is saved that would otherwise have been lost. If you'd like to dig deeper, you can explore the foundational research on the programme's effectiveness to learn more.

Navigating the NHS breast screening guidelines can feel a bit daunting, but it's actually a very straightforward system designed to take the guesswork out of your health. Think of it as a proactive check-in that comes directly to you, making sure you get the care you need at the right time.
The national programme is built to give everyone equal access to this life-saving check. It's like a scheduled service reminder for your car; the NHS tracks when you're due and sends an invitation right to your door, no matter where you live in the UK.
Your first letter from the NHS Breast Screening Programme will pop through your letterbox sometime between your 50th and 53rd birthdays. This is your official invitation to book your first mammogram within the national system.
Once you’re in the programme, you'll be invited back for screening every three years until you turn 71. The letter will have everything you need to know, including the location of your appointment and how to confirm or reschedule it.
These appointments usually happen at a dedicated breast screening centre or in a mobile unit that visits local communities, making it as easy as possible to attend.
The NHS focuses its automatic invitations on women aged 50 to 70. This isn’t an arbitrary number; it’s based on the fact that the risk of developing breast cancer goes up significantly with age, with most cases occurring in women over 50.
The three-year gap between screenings is also carefully calculated. It's a balance struck from extensive evidence about how quickly cancers can develop and become detectable, ensuring the programme catches them early without causing unnecessary procedures or radiation exposure.
The NHS Breast Screening Programme systematically invites women aged 50 to 70 for a mammogram every three years. This structured, evidence-based approach is fundamental to the UK's strategy for early cancer detection and improved treatment outcomes.
This system is a real cornerstone of public health in the UK. In England alone, the programme is run by 80 dedicated Breast Screening Units, all working together to provide free screening and any follow-up care needed. While the core age range is set, there's an ongoing trial looking at the benefits of expanding it to include women from 47 to 73. You can read more about the systematic approach of the NHS programme and how it’s constantly being refined.
So, what happens when you pass your 71st birthday? This is a common point of confusion, but the answer is simple: you are still entitled to free screening. The automatic invitations stop, but your access doesn't.
The responsibility just shifts from the NHS to you. Instead of waiting for a letter, you’ll need to proactively contact your local breast screening unit or chat with your GP to get an appointment booked in. It’s a small but important step in continuing to look after your health.
Why do the invitations stop?
The decision is based on a careful assessment of the overall benefits versus potential harms for this age group. However, the NHS absolutely supports a woman’s choice to continue with screening.
To make things clearer, here’s a simple table breaking down the standard timeline for women at average risk.
This table outlines the standard screening journey for women at average risk within the NHS programme.
Understanding these breast cancer screening guidelines is the first step toward taking an active role in your health. The system is designed to catch cancer early, right when treatment works best. By knowing when you’ll be invited and what your options are, you can make confident, informed decisions for years to come.
For most women, the standard three-year screening schedule is a solid safety net. But breast cancer doesn’t play by the same rules for everyone. A family history of the disease, specific genetic markers, or even certain medical treatments from your past can significantly raise your risk, meaning a more watchful approach is needed.
Think of it like this: your family car gets its annual MOT, and that’s usually enough. A high-performance racing car, however, needs more frequent, specialised checks to stay in peak condition. It’s the same logic for women at a higher risk of breast cancer—they need a more personalised screening plan to catch any potential issues as early as humanly possible.
Understanding what actually puts you in a higher-risk category is the first step. It’s what empowers you to have a proactive conversation with your GP and get the right level of care.
The NHS doesn't take a one-size-fits-all approach here. Instead, your risk is often categorised based on your lifetime chance of developing breast cancer, which is calculated using several crucial factors.
After a detailed assessment, your GP or a genetics specialist might place you in a moderate or high-risk group. This classification is what opens the door to a more intensive screening programme.
For those identified as having an increased risk, the NHS offers a surveillance programme that looks quite different from the standard schedule. It’s all about being proactive and spotting changes at the earliest possible moment.
Women with a moderate (17-29%) or high (30% or more) lifetime risk of breast cancer are offered enhanced screening under NICE guidelines. This typically involves annual screening from age 35, or starting five years younger than the age your youngest relative was when they were diagnosed (but not before 30).
This protocol is crucial, especially when you consider around 55,000 women in the UK are diagnosed with breast cancer every year. These enhanced pathways are proven to improve outcomes, and if you’re interested, you can explore the research on enhanced screening and survival rates to see the data for yourself.
The screening itself is also more comprehensive. It often involves using a combination of tools to get the clearest possible picture of your breast health.
The infographic below shows the main screening methods used in breast health surveillance.
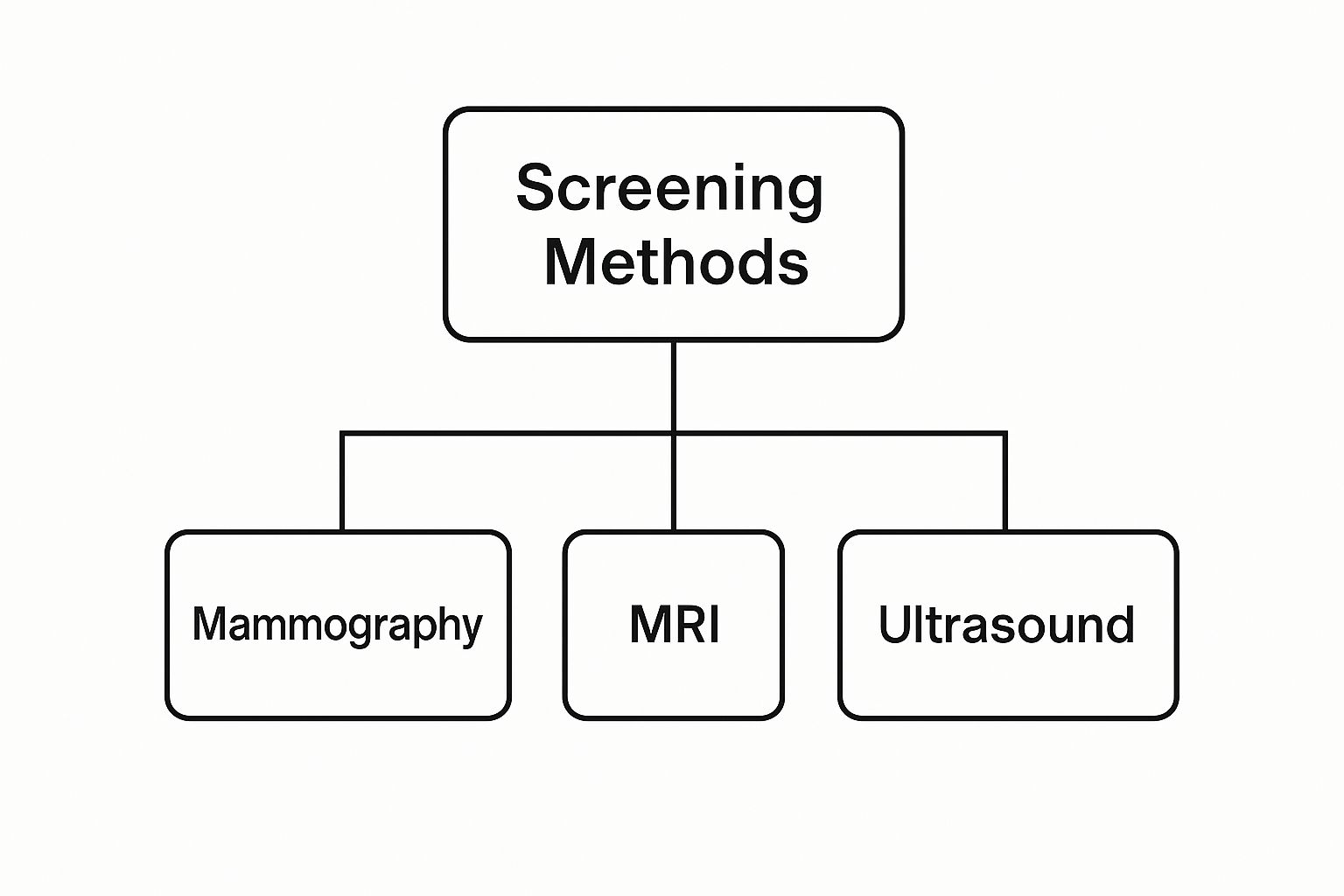
As you can see, mammography is the foundation, but it’s often supplemented by MRI and ultrasound for a deeper investigation, particularly in higher-risk situations.
For high-risk women, especially those who are younger and tend to have denser breast tissue, a mammogram on its own might not be enough. Dense tissue can sometimes hide small cancers on a standard X-ray, a bit like trying to find a white polar bear in a snowstorm.
This is where Magnetic Resonance Imaging (MRI) becomes an invaluable partner. An MRI uses powerful magnets and radio waves—no radiation—to create detailed, cross-sectional images of the breast. It’s particularly good at seeing through dense breast tissue to spot abnormalities.
For women in high-risk groups, the NHS often recommends annual MRI scans, sometimes starting as young as age 30, in addition to annual mammograms from age 40. This dual-imaging approach provides a far more sensitive and thorough check.
Combining these technologies lets us play to the strengths of both. A mammogram is brilliant at detecting tiny calcifications (which can be an early sign of cancer), while an MRI excels at identifying soft tissue masses that a mammogram might miss. Together, they create a much finer safety net, massively increasing the chances of early detection.
If you think your family history or other factors might put you at higher risk, it is vital to talk to your GP. They can assess your personal situation and, if needed, refer you to a genetics service or a family history clinic for a more detailed evaluation. Understanding your risk is the key to unlocking the right screening plan for you. It’s also important to be aware of the signs of other conditions; you can learn more about gynaecological cancers in our detailed patient guide. Being informed about your overall health puts you in the driver's seat of your own care.

For many people, the thought of a mammogram can bring up a mix of nerves and uncertainty. Knowing what’s going to happen, step by step, can make the whole process feel much less daunting. Think of this as a simple walkthrough of your appointment, from arrival to results.
The main goal is to demystify the experience and show you that it’s a quick, straightforward health check. While there might be a few moments of discomfort, they’re very brief. The peace of mind that comes from being proactive about your health is invaluable.
A little bit of prep can make your mammogram appointment go that much smoother. On the day, it's best to avoid using deodorant, antiperspirant, or any lotions on your chest and under your arms. Some of these products contain tiny metallic particles that can show up on the X-ray and mimic calcifications, potentially confusing the results.
What you wear also makes a difference. Choosing a two-piece outfit—like a top with trousers or a skirt—is a really practical idea. You’ll need to undress from the waist up for the procedure, so wearing separates just makes things easier and more comfortable.
A few simple tips to keep in mind:
When you're called in, a female radiographer—a healthcare professional specially trained in mammography—will guide you through everything. She'll ask you to stand in front of the mammogram machine, which is essentially a specialised X-ray unit.
The radiographer will position one of your breasts at a time on a clear plate. Then, a second plate will gently but firmly press down from above to flatten the breast tissue. This compression is crucial for two key reasons: it spreads out the tissue to get a clear image, and it holds the breast still to prevent any blurring.
You’ll typically have two pictures taken of each breast, one from the top and one from the side. The compression only lasts for a few seconds for each image. While it can feel a bit uncomfortable, it shouldn't be painful. The entire appointment usually takes less than 30 minutes, and the mammogram itself is over in just a few minutes.
A mammogram is a very quick procedure. The compression might feel strange or uncomfortable, but it’s over in seconds and is vital for capturing a high-quality image that allows radiologists to spot even the smallest changes.
Once your mammogram is done, you can get dressed and carry on with your day. Your X-ray images will be carefully examined by at least two expert radiologists who are looking for any signs of abnormalities.
The next step is waiting for your results, which are usually sent by post to you and your GP within two weeks. For the vast majority of women—around 96 out of every 100—the result will be normal, and you’ll simply be invited back for your next routine screening in three years.
Sometimes, though, the results aren't perfectly clear, and you might be called back for further assessment. It’s so important to remember that this does not automatically mean you have cancer. In fact, most women who are recalled are found to have nothing wrong at all.
A recall can happen for a few reasons:
If you are called back, you'll be invited to a specialist assessment clinic. There, you might have more detailed mammograms, a breast ultrasound, or in some cases, a biopsy, where a small tissue sample is taken for analysis. This thorough process ensures any concerns are fully investigated, giving you a definitive answer and a clear path forward.
Getting to grips with the breast cancer screening guidelines is only half the story. To make a decision that feels right for you, it’s vital to have a balanced view, weighing the incredible life-saving power of screening against its real-world limitations. Let's be clear: no medical test is perfect, and mammography is no exception.
The biggest benefit is simple and powerful: early detection saves lives. Screening mammograms are designed to find cancers when they are tiny, often long before they can be felt. Catching cancer at this early stage means treatment is usually less invasive and has a much higher chance of success.
Think of it like spotting a small ember before it can grow into a wildfire. An early-stage cancer is a contained problem, often treatable with more straightforward surgery and less aggressive therapies. This not only improves survival rates but also makes a huge difference to a person's quality of life during and after treatment.
This proactive approach is the very heart of the NHS screening programme. It's a strategy backed by solid evidence, proven to reduce the number of women who die from breast cancer, making it one of the most important public health initiatives in the UK.
One of the most common worries is the risk of a "false positive." This is when a mammogram shows something that looks like it could be a problem, leading to a recall for more tests, but it turns out to be nothing. It’s important to know that being called back is relatively common—around 1 in 10 women might be recalled for a closer look.
For the vast majority of those recalled, everything turns out to be fine. However, the experience itself can be incredibly stressful. That wait for more tests and the final results can cause a lot of anxiety.
A false-positive result isn't a mistake; it's a sign that the screening process is being thorough. The follow-up tests are just a necessary step to make sure any potential concerns are properly investigated and ruled out.
Interestingly, this experience can sometimes put women off attending future screenings. Studies have shown the anxiety of a false-positive can lead some to delay or skip their next mammogram. This is why understanding the process is so crucial for staying on top of your long-term health. Preventive checks, like the ones detailed in our guide to the role of blood testing in healthcare, work best when they're done consistently.
A more complex issue to consider is overdiagnosis. This happens when screening finds a very slow-growing cancer that would never have caused any harm or symptoms during a person's lifetime. The problem is, it's currently impossible to tell which cancers will become life-threatening and which won't, so they are all treated.
This means some people may go through treatments like surgery, radiotherapy, or hormone therapy for a cancer that would never have affected them. It’s a significant point to consider, and experts are constantly working to find better ways to distinguish between aggressive and slow-growing cancers to minimise this issue.
To help you see the full picture, here's a straightforward look at the key arguments for and against regular breast screening.
Ultimately, the decision to screen is a personal one, but it's based on a public health strategy that has saved thousands of lives.
Beyond screening, it's also vital to be aware of how daily choices, such as alcohol consumption, influence your overall health. For more on this, you can read about understanding lifestyle factors that impact cancer risk.
By being aware of both the incredible benefits and the potential downsides, you can approach your screening invitations with confidence, knowing you are making a well-rounded and proactive choice for your health.
Even with the national programme laid out, it’s completely normal to have questions that are a bit more personal. Everyone's health journey is different, and when it comes to something like breast cancer screening, specific worries often pop up. Here, we tackle some of the most common queries we hear from patients.
The aim is to give you clear, reassuring information so you can feel confident and in control of your breast health.
If you're younger than the routine screening age but have a concern, the single most important thing you can do is practise breast awareness. This just means getting to know what’s normal for your breasts so you can spot anything different, and spot it quickly. Check regularly for new lumps, nipple changes, or anything that feels unusual for you.
If you do notice a change, don't put it off. The right move is to contact your GP immediately. They are your first port of call and can assess what’s going on. If needed, they’ll refer you for further tests like a mammogram or ultrasound. To learn more about that process, have a look at our guide on what to expect when referred for breast cancer assessment.
This is a very common and totally understandable worry. Let’s break it down.
First, the "pain" part. A mammogram needs to compress the breast for a few seconds to get a clear image. For some, this can be uncomfortable or briefly painful, but the feeling is over in a flash. The whole thing only takes a few minutes.
As for safety, mammograms use a tiny dose of radiation. The risk from this is incredibly small, especially when you weigh it against the massive benefit of catching cancer early. To put it in perspective, the radiation from one mammogram is about the same as the natural background radiation you’d get over a few weeks just by living your life.
A mammogram is a fast, safe, and effective screening tool. That moment of discomfort is a tiny trade-off for a test that can find cancer when it’s most treatable, dramatically improving outcomes.
Breast density is all about the mix of tissues in the breast—how much fibrous and glandular tissue there is compared to fatty tissue. You can’t see or feel it yourself; it’s something that only shows up on a mammogram. It's also very common, particularly in younger women.
The main issue with dense breasts is that both the dense tissue and potential cancers can look white on a mammogram. It’s a bit like trying to spot a snowball in a blizzard. Because of this, women with very dense breasts might be offered extra screening, like an ultrasound or MRI, to get a clearer picture.
Life happens, and appointments get missed. If this happens with your screening, don't stress—the important thing is to simply rebook it as soon as you can.
Just call the number on your original invitation letter. If you’ve lost it, you can contact your local NHS breast screening unit directly. Getting screened is one of the best things you can do for your long-term health, so it’s well worth the effort to get it back in the diary. When it comes to discussing results or personal concerns remotely, options like effective video conferencing for healthcare can also make follow-up conversations much easier.

If you are concerned about your health, book an appointment to see the team at The Vesey today.