.webp)
Deviated septum surgery, known as a septoplasty, is a procedure designed to correct the crooked wall of cartilage and bone that sits between your nostrils. The entire goal is to improve airflow, dial down chronic congestion, and finally resolve those frustrating breathing difficulties. For many people, it’s the definitive solution when other treatments just haven't cut it.
Think of your nasal septum as a thin, internal wall separating your two nostrils. Ideally, this wall is perfectly straight, letting air flow evenly through both sides. But for a huge number of us, this wall is off-centre—or "deviated."
A deviated septum can be something you’re born with, or it can be the result of a knock to the nose later in life. A minor deviation might not cause any trouble at all, but a more severe one can act like a permanent roadblock in one of your nasal passages, leading to a whole host of persistent and annoying symptoms.
Living with a deviated septum often means dealing with much more than just a stuffy nose. That restricted airflow can cause a cascade of issues that really start to impact your daily life and overall well-being. Recognising these specific signs is the first step toward getting a proper, lasting solution.
Common symptoms include:
The real clue is when these symptoms are chronic and just don't get better with standard treatments like nasal sprays or allergy medicines. If you constantly feel blocked up on one side, it strongly suggests a structural issue rather than just temporary inflammation.
Deciding to go ahead with deviated septum surgery usually happens after other, less invasive treatments have failed to bring any real relief. If you've already tried decongestants, antihistamines, and nasal steroid sprays without much success, and your symptoms are still affecting your quality of life, it’s probably time to speak with a specialist.
It's so important to understand the different ways you can treat these persistent issues. You can learn more about surgical solutions for nasal blockage to see if it lines up with what you're experiencing. The goal of surgery isn't just to straighten the septum for the sake of it; it's about restoring proper function and giving you back the ability to breathe freely, day and night.
If you're wondering whether your symptoms point towards a structural issue like a deviated septum, this checklist can help clarify things. Use it to assess what you're experiencing and decide if it's time to have a chat with a doctor.
This checklist isn't a substitute for a medical diagnosis, of course, but if you're ticking several of these boxes, a consultation with an ENT (Ear, Nose, and Throat) specialist is a very sensible next step. They can properly diagnose the issue and talk you through all the available options.
Figuring out that your chronic breathing issues might stem from a deviated septum is the first big step. The next is getting a formal diagnosis, and in the UK, that journey almost always starts with a visit to your local GP. Think of this initial chat as the gateway to getting specialist care.
Going into this appointment prepared can make a huge difference. Your GP needs the full picture: what are your symptoms, how long have you had them, and how much are they affecting your day-to-day life? Be ready to talk about everything from a constantly blocked nose and snoring to recurring sinus infections.
You're essentially building a case for a referral. The more clearly you can explain your struggles, the easier it is for your GP to see that this is probably a structural problem needing an expert eye.
Before you go, try keeping a simple symptom diary for a week or two. Nothing complicated – just jot down when your nose feels most blocked, how it’s messing with your sleep, and any other related issues like facial pressure or nosebleeds.
During the consultation, your GP will do a basic physical check. They’ll likely use a small, lighted instrument to have a quick look inside your nostrils and get a first impression of your nasal passages. While a major deviation might be obvious, a definitive diagnosis needs a much closer look.
This is your moment to proactively ask for a referral to an Ear, Nose, and Throat (ENT) specialist. Explain that you've already tried things like nasal sprays without any real relief and that you believe your symptoms are serious enough for an expert opinion.
Once your referral comes through, you'll have an appointment with an ENT specialist. This consultation is far more thorough and is usually where the final decision about deviated septum surgery is made. The specialist will carry out a detailed examination to confirm the diagnosis and also rule out other potential culprits for your symptoms, like allergies or nasal polyps.
The key tool for this is a nasal endoscope – a very thin, flexible tube with a tiny camera and light on the end.
A nasal endoscopy might sound a bit daunting, but it's a quick and generally comfortable procedure done right there in the clinic. It gives the specialist a crystal-clear, magnified view of your entire nasal cavity and the full length of the septum, which just isn't possible with a simple light.
This detailed view is essential. It allows the surgeon to see the exact location and severity of the deviation, check the health of your nasal lining, and spot if other problems, like enlarged turbinates, are adding to the blockage. To get a better idea of what to expect, you can learn more about what a full ear, nose, and throat (ENT) assessment involves.
After the examination, the specialist will sit down with you to discuss what they've found. They'll confirm whether a deviated septum is the main reason for your breathing difficulties and talk through whether surgery is the right move for you. The decision really boils down to a few key things.
Key criteria for recommending surgery:
The specialist will clearly lay out the potential benefits of a septoplasty against the risks, making sure you have all the information you need to make a confident, informed decision about going ahead with surgery.

It’s completely normal to feel a bit apprehensive before surgery, but understanding what’s involved in a deviated septum surgery can make a world of difference. The best way to picture it is like a skilled renovation. Your surgeon is an expert builder, carefully straightening a crooked internal wall to improve airflow, all without leaving a single mark on the outside.
This procedure, known as a septoplasty, is all about precision and subtlety. It’s performed entirely through the nostrils, which means no external cuts, no visible scars, and absolutely no change to the shape of your nose. The focus is purely internal—to fix the structure so you can breathe freely again.
On the day, the first step is a general anaesthetic. This ensures you’re completely asleep and comfortable, allowing the surgical team to work meticulously without causing you any discomfort.
Once you’re comfortably asleep, the surgeon gets to work. The whole process is methodical and precise, designed not just to straighten the septum but to do so while preserving the delicate structures of your nose.
Here’s a breakdown of the key stages:
Think of it like a tailor altering a suit. The surgeon isn't removing the entire structure; they’re making precise adjustments, trimming and reshaping it to create a perfect, functional fit for your airway.
Sometimes, a deviated septum is only one piece of the puzzle. Your surgeon might find that other structures inside your nose, called turbinates, are also enlarged and blocking your breathing. Turbinates are small, bony structures covered in soft tissue that help warm and humidify the air you breathe.
If they’re chronically swollen, they can obstruct airflow even after the septum is fixed. In this case, your surgeon may recommend a turbinate reduction at the same time as your septoplasty. This combination is very common because it tackles multiple sources of blockage in one go, greatly improving your chances of achieving clear, easy breathing.
If you’re also considering changes to the appearance of your nose, a septorhinoplasty procedure may be discussed instead.
Septoplasty is a routine and well-established procedure here in the UK. Between 2012 and 2019, a total of 158,031 septoplasties were performed, mostly on adults and more commonly on men. It’s a significant and effective operation that makes a real difference to people’s quality of life.
Getting ready for deviated septum surgery isn't just about the day itself; it's about setting the stage for a calm, comfortable recovery. A bit of planning beforehand makes a world of difference, letting you focus entirely on healing instead of scrambling with last-minute details.
Think of it like preparing your home for a long weekend away. You get everything sorted first so you can relax properly. This means organising the practicals, like getting a lift home, and following your surgeon’s pre-op instructions to the letter—they’re there to keep you safe and minimise risks.
In the week or two leading up to your operation, a clear plan can help manage any pre-surgery nerves and put you firmly in control.
Here’s what to prioritise:
One of the most critical steps is stopping any medications or supplements that can thin the blood and increase bleeding risk. This includes things like aspirin, ibuprofen, and even some herbal remedies like fish oil. Your surgical team will give you a specific list of what to avoid and when.
Follow this simple checklist in the weeks and days before your surgery to ensure everything is in order for a smooth process.
This checklist is your roadmap to a hassle-free experience, taking the guesswork out of the final few days.
The final 24 hours are all about following the last few crucial instructions from your medical team. This will almost certainly include fasting—no food or drink (not even water) for a set number of hours before your procedure. It's a non-negotiable safety measure for anaesthesia.
Use this time to pack a small bag for the hospital with a few essentials. Comfortable, loose-fitting clothes for the journey home, a phone charger, and maybe something to read are all you’ll need. Do one last check of your recovery space at home to make sure everything you might want is within arm's reach. For a more detailed guide, our article on how to prepare for surgery has some excellent extra tips.
By following these steps, you'll walk into your surgery day feeling organised and confident. You’ve done the prep work, and now you can look forward to the result: breathing clearly and freely for years to come.
Knowing what to expect after your deviated septum surgery is key to a smooth, confident healing process. Recovery isn't an overnight fix; it's a gradual journey. This week-by-week guide breaks down the key milestones, helping you manage expectations and navigate the path to finally breathing clearly.
The timeline below gives you a sense of how preparation begins long before your actual surgery day.
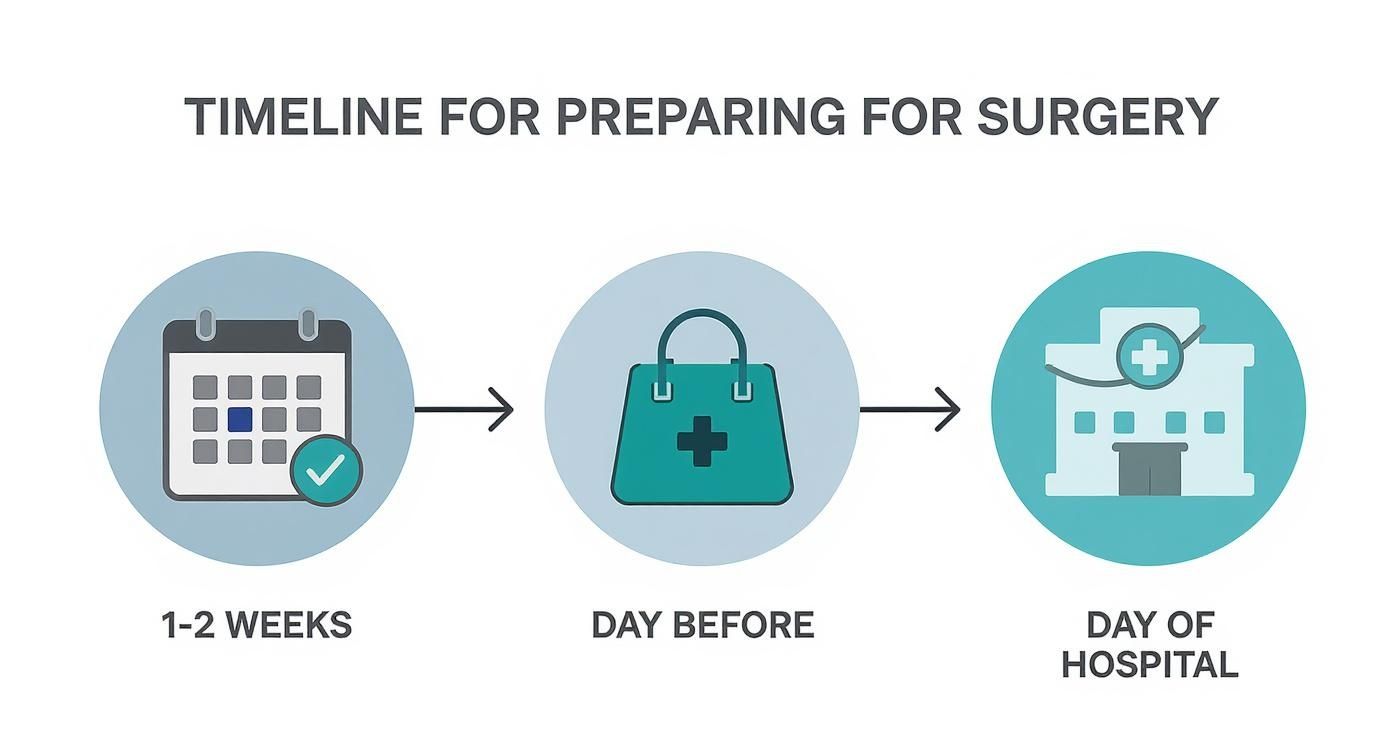
As you can see, getting ready starts weeks in advance, moving from early arrangements to specific tasks on the day itself.
The first week is definitely the most intense part of recovery. You'll likely feel very congested, a bit like having a nasty cold. This is completely normal—it’s just your body’s reaction to internal swelling and any splints or packing your surgeon placed inside your nose to support the newly straightened septum.
Your number one job during these first few days? Rest.
Keep your head elevated, even when you sleep, by propping yourself up on a few pillows. It’s a simple trick, but it’s one of the most effective ways to keep swelling down and reduce that feeling of pressure in your nasal passages.
You might have some mild discomfort and a bit of light bleeding or discharge for the first 24 to 48 hours. Your surgeon will give you a clear plan for managing any pain, which is usually handled with over-the-counter pain relievers. While there's general guidance on when to use ice or heat for discomfort, always stick to your surgeon's specific advice after an operation like this.
A critical rule to follow will be to avoid blowing your nose. It feels counterintuitive, but it can easily disrupt the healing tissues. Instead, use the saline nasal sprays your doctor recommends to gently clear and moisturise your nasal passages.
By the second week, you should really start to feel a difference. That heavy congestion will begin to ease up as the initial swelling subsides. Many surgeons remove the internal splints or packing around the end of the first week or early in the second, and that often brings an immediate sense of relief and much better airflow.
This is the time to start reintroducing some light activity into your daily routine. A gentle walk is great, but it’s crucial to continue avoiding anything strenuous.
Things you absolutely must steer clear of at this stage include:
Most people feel ready to return to a desk-based job by the end of the first or second week, as long as it isn’t physically demanding.
Once you hit the fourth week, you’re in the home stretch. Most of the major swelling will be gone, and your breathing should feel clearer and more effortless than it has in years. During your follow-up appointments, your surgeon will check on your healing and will likely give you the green light to resume most of your normal activities, including more intense exercise.
The key is to listen to your body. Ease back into things gradually. Even though you'll feel much better, the deep healing of cartilage and bone actually continues for several months. You’ll probably notice subtle but steady improvements in your breathing during this time.
The procedure has a strong track record of success. For example, the UK-based NAIROS trial showed that septoplasty leads to a huge improvement in nasal blockage symptoms six months after surgery when compared to non-surgical options. The study really focused on patients with moderate to severe symptoms, confirming that deviated septum surgery is most beneficial for those who are struggling the most.
By the six-week mark, the vast majority of patients feel fully recovered and are finally enjoying the full benefits of their decision to have a septoplasty.
Deciding to have surgery is a big step, and a septoplasty is no different. It’s all about balancing the life-changing potential against some small, but important, risks. For most people, a successful deviated septum surgery is genuinely transformative, unlocking a quality of life they haven’t had for years.
The most immediate and obvious benefit? Clear nasal breathing. Imagine the simple relief of taking a full, deep breath through both nostrils without a second thought. This has a knock-on effect, leading to much better sleep quality as the nightly struggle for air—the cause of snoring and restless nights—is finally over. Many patients also tell me they get far fewer sinus infections, because proper drainage stops the mucus build-up that causes those recurring problems.
While septoplasty is a very safe and routine operation, it’s only right to be aware of potential complications, however rare they may be. A skilled surgeon minimises these risks, but being fully informed is part of the process.
Potential risks can include:
Your surgeon will go over all of these with you in detail, making sure you feel completely comfortable and confident before going ahead.
In the UK, there are two main routes to getting this surgery: through the NHS or via private healthcare. The right choice often comes down to the urgency and severity of your symptoms, as well as your personal circumstances.
The National Health Service (NHS) funds septoplasty when there’s a clear functional need. This means the surgery gets the green light if a deviated septum is causing significant medical issues like severe nasal blockage, chronic sinusitis, or contributing to sleep apnoea. It is not performed for purely cosmetic reasons.
The main hurdle on the NHS pathway can be the waiting times, which can be quite long from your initial GP referral to the day of your operation.
On the other hand, opting for private healthcare offers a much quicker path to treatment. You can typically see a specialist and have your surgery scheduled within weeks, not months. If this is something you're thinking about, you can learn more about what private healthcare entails and see how it provides faster access to the care you need.
Septoplasty is a common and highly effective procedure in the UK. In the 2019-20 period alone, around 16,700 septoplasties were carried out in England, which shows just how frequently this solution is used to fix nasal obstruction. Major studies have consistently found that surgery delivers better results than just medical management for people with moderate to severe symptoms. Read the full research about these findings. The evidence is clear: for many, surgery is the most reliable way to find lasting relief.
Even after getting the facts, it’s completely normal to have a few more questions pop into your head. Here are some straightforward answers to the most common things patients ask about deviated septum surgery, designed to help you feel confident and ready.
This is probably the number one question we hear, and it’s an important one. The short answer is no. A standard septoplasty is purely a functional operation. Its only goal is to straighten the wall inside your nose to help you breathe better.
The entire procedure happens inside your nostrils, so it will not change the external shape or appearance of your nose. If you do want to make cosmetic changes, that’s a different procedure called a septorhinoplasty. This combines the functional fix of a septoplasty with the aesthetic work of a rhinoplasty, tackling both breathing and appearance in one go.
Most people are pleasantly surprised. The feeling is less about sharp pain and more about pressure and stuffiness, a lot like a heavy head cold.
Any actual pain is usually quite mild and easily handled with the pain relief your surgeon prescribes for the first few days. After that, over-the-counter options are typically all you’ll need. For most, the biggest challenge is simply the nasal congestion from swelling, which gets a lot better after the first week.
This really comes down to what you do for a living.
It’s always smart to plan for a little more downtime than you think you’ll need. Rushing back to work can set your recovery back, so giving your body that extra time to rest is crucial.
This is where a bit of patience is needed. Right after the surgery, you’ll actually feel more congested because of the swelling. That’s totally normal. Most patients start to notice a real improvement in their breathing about one to two weeks after the operation, usually after the initial swelling has gone down and any internal splints are removed.
But the healing doesn't stop there. Your body continues to heal on the inside for several months. You should expect your breathing to get progressively better over the next three to six months as all that deep swelling fully resolves. That's when you'll experience the final, lasting result.
At The Vesey, our dedicated ENT specialists are here to guide you through every step of your journey to better breathing. If you're ready to find a lasting solution for nasal obstruction, we invite you to book a consultation and discuss your options with one of our experts. Learn more at https://www.thevesey.co.uk.

Expert ear, nose an throat surgery at The Vesey