.webp)
Gastric sleeve surgery, known in medical circles as a sleeve gastrectomy, is a procedure designed to help people achieve significant and lasting weight loss. It involves carefully removing a large section of the stomach, leaving behind a much smaller, banana-shaped pouch.
This isn't just about making the stomach smaller; it’s a powerful tool that changes your relationship with food and hunger itself.

Think of your stomach like a large, stretchy bag that can hold a lot of food. Gastric sleeve surgery effectively swaps that big bag for a much smaller, less expandable one. This simple change drives weight loss in two key ways.
The first is purely mechanical. By removing about 75-80% of the stomach, the new pouch that's left behind can only hold a fraction of what it used to. You physically can't eat as much, so you feel full much faster, which naturally slashes your calorie intake.
The second, and perhaps more profound, change is hormonal. The part of the stomach that's removed happens to be the primary production centre for ghrelin—often called the "hunger hormone."
With ghrelin production drastically reduced, most people find their appetite plummets. This hormonal reset makes it far easier to stick to a healthier diet without battling constant hunger pangs.
For a quick overview of what the procedure entails, here's a simple breakdown.
This table summarises the core mechanics, but deciding if it's the right path requires a much deeper conversation.
A gastric sleeve isn't a cosmetic procedure or a quick fix; it's a serious medical intervention for those whose health is at significant risk due to their weight. It's generally considered for individuals who meet specific criteria:
The ultimate goal is to offer a lasting solution for people who need it most. This surgery, a specialised procedure within the field of general surgery, provides the foundation for building a healthier, more active life from the ground up.
Deciding to have gastric sleeve surgery is a massive step, and frankly, it isn't for everyone. Here in the UK, the guidelines are quite specific, making sure the surgery is offered to people who genuinely need it and are truly ready for the road ahead. It’s a process that involves taking a close look at your physical health, your past experiences with weight loss, and whether you're psychologically prepared for such a significant change.
The starting point for this conversation is almost always your Body Mass Index (BMI). It's a straightforward calculation that gives a picture of your weight in relation to your height. While it's not the be-all and end-all, it’s the first crucial piece of information doctors use.
Generally, potential candidates fit into one of two main groups. The first group includes anyone with a BMI of 40 or higher, which is what doctors call severe obesity. At this level, the health risks from the weight itself are serious enough to consider surgery. The second group is for those with a BMI between 35 and 40 who are also dealing with at least one major health problem linked to their weight.
These related health issues, which doctors often call co-morbidities, are a huge part of the assessment. They are medical conditions that are either directly caused by or made much worse by excess weight. Having one or more of these can really strengthen the case for going ahead with surgery.
Some of the most common co-morbidities we see are:
When these conditions are present, it’s a clear sign that your weight is already damaging your health, which makes finding a lasting solution all the more urgent.
Qualifying for a gastric sleeve is about so much more than just hitting a certain BMI. A huge part of the process is figuring out if you're mentally and emotionally prepared for the lifelong adjustments the surgery requires. This isn't just an operation; it's a firm commitment to an entirely new lifestyle.
Surgeons and their teams need to see that you understand the surgery is a tool, not a cure-all. Your own commitment to a healthier way of life is what will truly determine your success in the long run.
Before surgery is even on the table, it's wise to have explored all the other options out there, including prescription weight loss medications. In fact, showing that you've made a real, documented effort to lose weight through traditional methods is a must. This usually means you’ve spent at least 12 months trying to manage your weight with a supervised plan involving diet, exercise, and lifestyle changes, but without seeing the results you need.
In the UK, the NHS eligibility criteria for 2025 are very clear-cut. Patients generally need a BMI of 40+, or a BMI between 35 and 40 alongside a significant weight-related health problem. You also need to be psychologically ready, typically between 18 and 65 years old, and have maintained a stable weight for three months before your assessment. These strict rules are there to ensure NHS resources go to patients with a clear clinical need who are fully prepared for what's involved.
A full team, including dietitians and psychologists, will work with you to make sure you’re ready. If you're weighing up your options, looking into a private weight loss service can offer a thorough evaluation and a tailored support plan to help you decide on the best way forward for your health.
Thinking about gastric sleeve surgery can feel overwhelming, but understanding what the process actually involves, step by step, makes it all feel much more manageable. It’s not just about one day in the operating theatre; it’s a carefully planned journey designed to get you physically and mentally ready for the changes to come.
This journey starts well before surgery day, with detailed conversations and medical checks to make absolutely sure this is the right and safest path for you.
Your first real step is an in-depth consultation with a bariatric surgeon and their team. This isn't just a quick chat. It's a comprehensive evaluation where you'll go through your weight history, what you've tried before to lose weight, and any health conditions you might have. Think of it as a two-way conversation—it’s your chance to ask every question that's on your mind and for the team to get a crystal-clear picture of your health.
After that initial meeting, you'll go through a series of medical tests. These are non-negotiable, as they ensure you’re fit for surgery and flag any potential risks. You can generally expect:
This pre-operative stage is all about laying a solid foundation for a successful outcome.
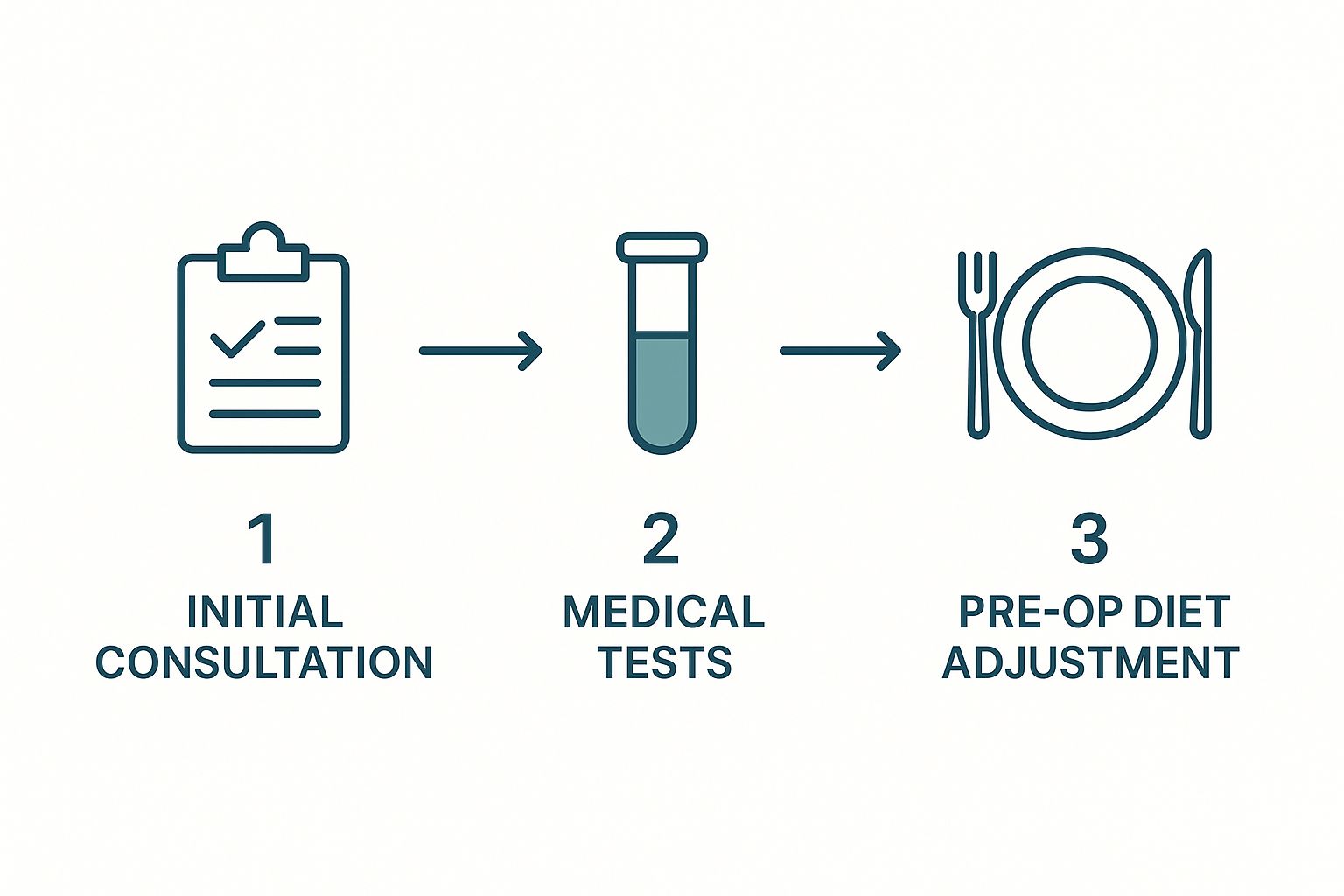
As you can see, the process moves logically from initial chats to detailed assessments and finally to dietary changes. It’s all about making sure every box is ticked before the day of your procedure.
Once you've been given the green light for surgery, the preparation phase kicks into high gear. A crucial part of this is the pre-operative diet, which typically starts two to four weeks before your surgery date. This is usually a strict low-calorie, low-carbohydrate, and high-protein plan, often relying on meal replacement shakes.
Why is this so important? The main goal is to shrink your liver. A large liver can physically get in the way during surgery because it sits right next to the stomach. A smaller liver gives the surgeon a much clearer view and better access, which makes the whole operation safer and more straightforward. For a deeper dive into this stage, our guide on how to prepare for surgery has plenty of helpful tips.
On surgery day, you’ll be admitted to the hospital. After handling the final bits of paperwork and having a chat with the anaesthetist, you'll head to the operating theatre. The procedure is done under general anaesthesia, so you’ll be completely asleep and won't feel a thing.
Surgeons almost always use a minimally invasive approach called laparoscopic surgery, which you might have heard of as 'keyhole' surgery.
Instead of one large cut, the surgeon makes a few small incisions in the abdomen. A tiny camera (the laparoscope) and special surgical tools are passed through these small openings to perform the operation.
The surgeon then carefully removes about 80% of your stomach, shaping the remaining part into a narrow tube or 'sleeve' with a surgical stapler. The whole thing is surprisingly quick, usually taking between 60 and 90 minutes.
This keyhole method is a game-changer. Because the incisions are so small, patients experience less pain, have a shorter hospital stay (typically one or two nights), and recover much faster than with old-school open surgery. Afterwards, you'll be taken to a recovery room where the team can monitor you closely as you wake up from the anaesthesia.

Many people see the surgery itself as the main event, but I always tell my patients that it's the starting line, not the finish. The real journey begins once you're home. This is where you'll build a completely new relationship with food and reshape your daily life as your body heals.
Your first few weeks will be dedicated to recovery. Expect to feel tired and sore—that's perfectly normal. The main focus here is simply on resting, staying hydrated, and gently reintroducing your digestive system to nourishment. It's a slow, steady process that demands patience and sticking closely to the plan your surgical team has laid out.
Your diet after surgery isn't something you can just jump back into. It progresses through several carefully planned stages. This gradual approach is absolutely vital for protecting your healing stomach, preventing complications, and letting your body adapt. Trying to rush things can lead to pain and serious setbacks.
It all starts with liquids. For the first week or two, your world will revolve around clear fluids like water, broth, and sugar-free drinks. This gives your new stomach a chance to heal without any stress. After that, you'll slowly progress to thicker liquids like protein shakes and smooth soups.
The dietary progression is a cornerstone of a successful recovery. Below is a simplified timeline of what you can generally expect as you move from liquids back to solid foods.
Each phase is a crucial stepping stone. This structured approach isn't just about healing; it's about re-learning how to eat for your new anatomy, setting you up for long-term success.
This new way of eating isn't a temporary diet; it's a permanent lifestyle. Your smaller stomach requires you to eat small portions, chew food thoroughly, and eat slowly to avoid discomfort and ensure you're getting the nutrients you need.
For anyone looking to be meticulous about their diet, exploring detailed reviews of food diary app options can be a massive help in finding the right tool to track intake and progress.
Because you’ll be eating so much less, getting all the vitamins and minerals your body needs from food alone is no longer possible. This is a non-negotiable part of life after a gastric sleeve. You will be on a specific regimen of supplements for the rest of your life.
Your team will give you a precise plan, but it will almost certainly include:
Regular blood tests will become a normal part of your life. They’re essential for checking your nutrient levels and making sure your supplement plan is working. Skipping them is not an option, as it can lead to serious health problems like anaemia and osteoporosis down the line.
While the physical changes get all the attention, the emotional and mental adjustments are just as significant. The rapid weight loss can be both thrilling and incredibly disorienting. It’s very common to experience a kind of ‘mind-body’ disconnect as you get used to seeing a new person in the mirror.
Your relationship with food will be fundamentally rewired. So many of us use food for comfort, celebration, or social connection. Learning new, healthier coping mechanisms is a huge part of the process. I strongly encourage patients to connect with support groups or a psychologist to help navigate these powerful emotional shifts.
This journey is about so much more than weight. It’s about building a sustainable, healthy lifestyle that nurtures both your body and mind for the long haul.
Deciding on gastric sleeve surgery means taking a clear-eyed look at both sides of the coin. It’s a powerful procedure that can genuinely turn your health around, but like any major operation, it isn’t without its challenges. Having a balanced perspective is the only way to make a choice that’s right for your future.
The most obvious benefit, and the one everyone talks about, is significant and lasting weight loss. This is about so much more than fitting into smaller clothes; it’s about lifting a heavy physical burden that affects every part of your life. The weight that comes off after a gastric sleeve can be truly life-altering, giving you the freedom to move easily and get back to activities you may have been missing out on for years.
This physical change sets off a domino effect of incredible health improvements. Many of our patients see a remarkable reversal of conditions that are directly tied to obesity.
When the excess weight disappears, it has a direct, positive impact on many serious health problems. For a lot of people, this is the real reason they choose surgery. The improvements can be so profound that some conditions go into complete remission.
Here are some of the key health benefits we see time and again:
These health wins don’t just add up to a longer, healthier life—they give you a massive boost in your day-to-day energy and well-being.
While the benefits are compelling, you have to go into this with your eyes wide open to the risks. We can break these down into short-term complications from the surgery itself and longer-term issues that require lifelong attention.
In the immediate aftermath of any operation, there are risks. These include things like infection, bleeding, blood clots, or a bad reaction to the anaesthetic. A more specific risk with the sleeve is a leak from the staple line where the stomach was divided. This is a serious complication that needs immediate medical help.
While surgeons take every possible precaution to minimise these risks, they can never be completely eliminated. Your best defence is choosing an experienced surgical team and a reputable hospital.
Looking at the long term, a different set of challenges can crop up. Nutritional deficiencies are a big one. Because you're eating so much less, your body has a smaller window to absorb vitamins and minerals. Lifelong supplementation isn't just a suggestion; it's a medical necessity to prevent problems like anaemia or osteoporosis down the line. Other potential issues include developing acid reflux or, rarely, a narrowing of the stomach sleeve, known as a stricture.
Finally, we need to talk about weight regain. The gastric sleeve is an incredible tool, but it's not a magic fix. If old eating habits creep back in, it is possible to stretch the new stomach pouch and regain some of the weight. This is why ongoing support and a solid commitment to your new lifestyle are absolutely crucial for long-term success.
In the UK, around 5,000 bariatric surgeries are performed annually, with the gastric sleeve making up 55% of those procedures. Studies show that three years post-op, 41% of gastric sleeve patients have lost at least 50% of their excess weight. While these are fantastic results, it's worth noting that gastric bypass can sometimes lead to greater weight loss. Still, the sleeve is a vital and popular option, especially when a bypass isn't the right fit for a patient. You can discover more about these clinical findings to understand how the data shapes patient choices.

If you're in the UK and thinking about gastric sleeve surgery, one of the first hurdles is figuring out how to get it. There are really two main routes you can take: going through the National Health Service (NHS) or opting for private healthcare. These two paths are worlds apart, and each comes with its own realities you'll need to weigh up.
For most people, the journey starts with the NHS. It usually begins with a chat with your GP, who’ll see if you fit the very specific criteria. If you’re a potential candidate, you’ll then be referred to a specialist bariatric team for a much deeper assessment. The major plus here is that the cost is covered, but be prepared for a long road ahead.
There's no doubt the NHS provides fantastic care, but getting access can be a real test of patience. It’s often a case of a 'postcode lottery', where your location heavily influences your wait time.
Simply getting an initial consultation can take a long time, and the wait from that first appointment to your actual surgery can easily stretch into years. While the process is incredibly thorough to make sure you're ready, that lengthy wait can be a real source of frustration and worry.
It's a stark reality that access to care varies wildly across the country. In fact, research highlights that only a tiny fraction of people who are eligible for bariatric surgery – around 1% – ever actually have the procedure. Many find themselves waiting four years or more after they qualify, a period during which their health can sadly get worse. You can read the full research about these bariatric care gaps to get a clearer picture of the systemic challenges.
Faced with long delays or not quite meeting the strict NHS rules, many people decide to explore the private sector. The biggest draw here is, without a doubt, the speed. Wait times are slashed from years to mere weeks, meaning you can start your weight loss journey almost immediately.
Going private also gives you a lot more control. You get to choose your surgeon and the hospital, which can be very reassuring. Of course, this comes with a significant price tag. You can expect to pay anywhere from £8,000 to £12,000 for a gastric sleeve procedure. For a deeper dive into how this all works, our guide on what is private healthcare is a great starting point.
Private care packages often include comprehensive aftercare support, such as regular follow-ups with dietitians and psychologists, which are essential for long-term success.
There is a third option that’s become more common: medical tourism. This involves travelling abroad to countries like Turkey or in Eastern Europe where prices are much lower. While the cost savings are tempting, this route isn't without serious risks. If you run into complications once you’re back in the UK, getting follow-up care can be extremely difficult and expensive, often putting a strain on the NHS. It's crucial to carefully balance cost, speed, and safety before you make any decisions.
It's completely normal to have a head full of questions, even after you've researched the procedure, recovery, and risks. In fact, it's a good sign you're taking this seriously. Let's walk through some of the most common questions we hear from patients during their consultations.
This is, without a doubt, one of the top concerns people have, and it’s a perfectly valid one. When you lose a lot of weight quickly, it's very likely you'll have some excess skin, usually around your tummy, arms, and thighs.
How much loose skin you end up with really comes down to a few key things:
Building muscle through strength training can certainly help. Toning the muscles underneath gives the skin better support and can improve its appearance, but it won't make large amounts of excess skin disappear. Many patients do eventually decide to have cosmetic surgery to remove it, but that’s a conversation for much later, once your weight has been stable for some time.
Yes, absolutely. For many women, the weight loss that follows gastric sleeve surgery can actually boost fertility.
That said, we strongly advise waiting at least 12 to 18 months after your operation before you start trying to conceive. This isn't an arbitrary number.
There are two critical reasons for this wait. First, it gives your body a chance to find its new, stable weight, which creates a much safer environment for a developing baby. Second, it allows your body time to adjust to its new way of absorbing nutrients, reducing the risk of deficiencies that could impact both your health and your baby’s. When the time is right, you'll need to work closely with both your bariatric team and your obstetrician to ensure you're getting all the nutrition you need.
This is a common misconception. Once you're past the initial healing stages, very few foods are permanently "banned". The goal isn't about endless restriction; it's about learning to make smart choices that align with your new, smaller stomach.
However, you’ll quickly learn that certain foods just don't sit well anymore and are best avoided or eaten very carefully.
The usual suspects include:
The focus of your new life isn't on what you can't have, but on prioritising foods that give you the most bang for your buck—nutrient-packed lean proteins and fresh vegetables that nourish your body in smaller quantities.
At The Vesey, our dedicated team is here to guide you through every question and concern you may have on your weight loss journey. Explore our comprehensive weight loss services to learn how we can support you in achieving your health goals.

