.webp)
For most women, the hysteroscopy recovery time is wonderfully short. Many find they're back to their usual routine within a day or two.
If you’re having a simple diagnostic look-around, you can generally expect to be back on your feet within 24 to 48 hours. An operative hysteroscopy, where something like a polyp or fibroid is removed, naturally needs a bit more healing time, often up to two weeks.
Knowing what’s coming up after your procedure helps you plan and heal without worry. Think of it this way: a diagnostic hysteroscopy is like a minor medical MOT. You feel back to normal very quickly. An operative hysteroscopy, on the other hand, is more like a small internal repair job that just needs a little more downtime for your body to sort itself out.
A huge factor in your immediate recovery is the anaesthetic. Here in the UK, it really shapes that first day. Many women who have an outpatient procedure without a general anaesthetic are able to get back to their normal lives within 24 hours. If you’ve had a general anaesthetic, your body will need a few days of proper rest before you feel like yourself again.
To give you a clearer picture of the days ahead, this timeline breaks down the key stages you can expect during your recovery.
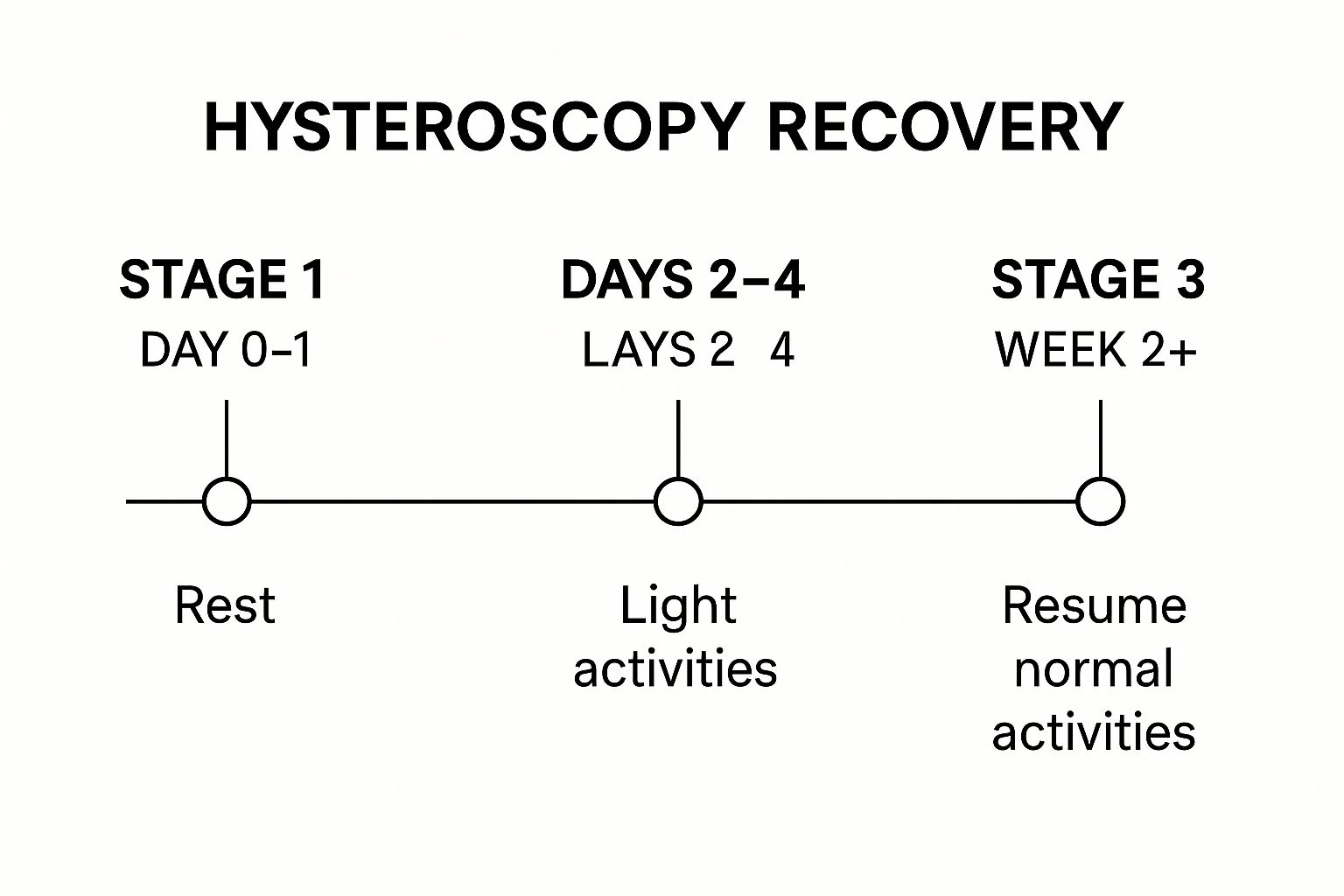
It’s a simple visual guide showing the natural progression from taking it easy at first, to slowly reintroducing light activities, and finally, getting back into your full swing.
Everyone’s journey is slightly different, depending on the exact nature of the procedure. For example, recovery after an endometrial polyp removal might involve a specific healing pattern as the lining of your womb settles down.
That said, most people will experience these key milestones:
To help you understand how the type of anaesthetic might influence your recovery, here’s a quick summary of what to expect.
This table gives a general idea of the recovery milestones, comparing procedures with and without general anaesthetic.
Remember, this is just a guide. The most important thing is to listen to your body and give it the time it needs to heal properly.

The first two days following your hysteroscopy are purely about rest and gentle self-care. Your body has just been through a medical procedure, and the most important thing you can do now is give it the time it needs to heal. Think of this period as a dedicated quiet time, allowing your body’s natural recovery processes to get started without any interruptions.
It’s completely normal to feel some mild, period-like cramping and see some light vaginal spotting or bleeding. This is just a sign that your uterus is healing as it should. How much you experience often depends on whether your procedure was a simple diagnostic look-around or a more involved operative one.
On the day of the procedure, your only job is to take it easy. If you had a general anaesthetic, you'll likely feel a bit groggy and will need to have someone with you for the first 24 hours. Even if you didn't, putting your feet up and resting is the best way to kickstart a smooth recovery.
Here’s what you might experience on the first day:
It's so important to remember that these initial symptoms are a perfectly normal part of the healing process. Your body is doing exactly what it's supposed to after a minor procedure, and these feelings won't last long.
Dealing with any discomfort is usually quite straightforward. Over-the-counter painkillers like paracetamol or ibuprofen are typically all you’ll need. For more ideas, exploring different effective pain relief strategies can give you some extra tools to manage any aches. Just be sure to follow the dosage instructions on the packet.
Make sure you drink plenty of water. Staying hydrated helps your body flush out any remaining anaesthetic and gives your healing a real boost. It’s also a good idea to stick to light, easily digestible meals for the first day, particularly if you feel a bit nauseous after a general anaesthetic. A bit of planning can make all the difference, and knowing how to prepare for surgery can make your recovery period feel much more manageable.
By the end of the first 48 hours, your hysteroscopy recovery time should be well underway. You'll probably find the cramping has eased off and any bleeding has become much lighter or stopped completely. Most women feel ready to get back to light daily activities, but remember to continue avoiding anything strenuous. The best advice is always to listen to your body – don't push it.

Once you’re past the first 48 hours, your body really gets down to the business of healing. This next phase, which lasts up to two weeks, is all about gradually easing back into your normal routine while giving your body the respect it deserves. The most intense part of your hysteroscopy recovery time is behind you; now, the focus shifts to a gentle return to daily life.
You should notice your symptoms getting progressively better day by day. The period-like cramping should have eased off significantly, if not vanished completely. Any light bleeding will also start to diminish, likely changing from a pinkish or red colour to a brownish discharge before it stops. These are all great signs that the lining of your uterus is healing just as it should.
Listening to your body is the absolute golden rule here. You might feel a lot better, but it's really wise to avoid launching straight back into strenuous activities. Think of it as gently applying pressure to the accelerator, not flooring it from a standing start.
I often get asked when it's safe to get back to certain things. Here's a general guide to help you navigate this period:
A key principle during this time is to avoid anything that could introduce an infection while the area is still healing. This is why waiting for the bleeding to stop is the standard advice for activities like swimming, using tampons, and having intercourse.
To ensure a smooth transition back to normality, you might consider looking into options for professional care after hospital discharge. This can be especially helpful if you live alone or if your procedure was on the more complex side.
For some, a hysteroscopy is just one part of a bigger treatment plan. For example, if your procedure was done to investigate issues ahead of another treatment, such as exploring options for endometrial ablation, then this recovery period is a crucial first step in your overall care journey.
By the end of that second week, most people feel they're completely back to their usual selves. You've navigated the main recovery phase and can confidently get back into your full routine. Just remember, this timeline is only a guide—your personal experience is what truly matters.

It’s completely normal for your hysteroscopy recovery time to look a little different from someone else’s. Think of it like recovering from a common cold; some people bounce back in a day, while others need a week to really shake it off.
Several personal factors come into play here. Understanding them can help you set realistic expectations for your own healing journey.
The single biggest factor is what the hysteroscopy was for. Was it purely to have a look around, or was a treatment carried out? This distinction is the key to figuring out your likely recovery path.
A diagnostic hysteroscopy is essentially an exploratory procedure. Since it’s just a look inside your uterus and no tissue is removed, the recovery is typically very fast. Most women feel back to normal within a day or two, with only minimal cramping or spotting.
An operative hysteroscopy, on the other hand, involves active treatment. This could mean removing polyps, fibroids, or taking a biopsy. Because this involves more direct interaction with the uterine lining, your body naturally needs a bit more time to heal. You can expect the recovery to be closer to one or two weeks.
The type of anaesthetic used also plays a big part in how you'll feel straight after the procedure.
Your overall health acts as the foundation for your recovery. Good general health can support a quicker healing process, while pre-existing conditions might mean you need a little more time to bounce back. This is an important part of your wider reproductive health.
Data from UK hospitals backs up this quick turnaround for many patients. Following outpatient procedures without general anaesthesia, recovery is often very rapid. Many women spend just 20 minutes in a recovery area before heading home the same day.
In fact, studies show that around 80% of women who have polyps or fibroids removed experience significant symptom relief, often within just days or weeks.
Ultimately, your personal hysteroscopy recovery time is a unique mix of these factors. Whether it was a simple check-up or a more involved procedure, giving your body the right amount of time to rest and heal is the most important step you can take. Listening to your body’s signals will always be your best guide.
While most people find their recovery from a hysteroscopy is smooth and straightforward, it's vital to know the difference between normal healing and a potential red flag. Your safety is always the top priority, and understanding the warning signs means you can act quickly if you need to.
Think of it this way: mild cramping and a bit of spotting are expected parts of the journey. But certain symptoms are more like a warning light on your car's dashboard—a clear signal to pull over and get things checked by a professional. Never hesitate to seek advice if you feel something isn't quite right.
Serious problems after a hysteroscopy are uncommon, but being prepared can give you real peace of mind. Pay close attention to how you're feeling and get in touch with your GP, the hospital clinic where you had the procedure, or NHS 111 if you notice any of the following.
These symptoms are not part of a typical recovery and need medical attention:
Your healthcare team would much rather you call with a concern that turns out to be nothing than have you wait at home while a potential issue develops. Trust your instincts—if it doesn't feel right, it’s always best to get it checked.
These symptoms can sometimes point to complications such as an infection or, in very rare cases, uterine perforation. An infection can happen if bacteria enter the uterus during or after the procedure, and it's important to treat it promptly with antibiotics to stop it from becoming more serious.
Some infections, if left untreated, can lead to conditions like pelvic inflammatory disease, which can have longer-term consequences. You can learn more about the signs of pelvic inflammatory disease in our detailed guide.
It’s worth repeating that complications are rare. Knowing the signs simply empowers you to take control of your health and make sure your recovery stays on a safe and healthy track.
Even with a clear timeline in mind, it's completely normal to have a few more specific questions buzzing around. Getting to grips with the practical, day-to-day details can make all the difference in feeling prepared and less anxious about your hysteroscopy recovery time.
Let's walk through some of the most common queries we hear, giving you straightforward answers to help you plan with confidence.
This really comes down to the type of anaesthetic you had. It’s all about keeping you, and everyone else on the road, safe.
If you had a simple diagnostic hysteroscopy with no anaesthetic, or just a local one, you’ll likely be fine to drive yourself home. You should feel alert and clear-headed.
However, if you had a general anaesthetic or sedation, you must not drive for at least 24-48 hours. Even if you feel perfectly okay, the anaesthetic can linger in your system, slowing your reaction times and affecting your judgement. It’s a legal and safety requirement, so be sure to arrange a lift home. Always listen to the specific advice from your hospital team.
Yes, it’s very likely your first period after the procedure will be a little out of the ordinary. Think of your uterus as a garden bed that’s just been neatly tended to – it needs a moment to settle back into its natural rhythm.
You might find your period arrives a bit earlier or later than usual. It could also be heavier, and you might notice more cramping than you’re used to. This is all part of the healing process as the uterine lining (the endometrium) recovers.
For most women, their cycle gets back to its familiar pattern within a month or two. This initial bumpy period is usually just a temporary blip while your body heals.
If you have any concerns, like extremely heavy bleeding, or if your periods don't settle down after a couple of cycles, it's always wise to have a chat with your GP.
It’s a good idea to put any long-distance travel on hold for a short while, especially flights. The main reasons are to ensure you’re comfortable and can easily get medical help if any complications pop up.
Sitting for long periods on a flight can slightly increase the risk of deep vein thrombosis (DVT), so it's best to be fully recovered first. If you have travel plans, make sure to discuss them with your doctor before your procedure to get personalised advice.
There are no strict dietary rules, but focusing on good nutrition and hydration can definitely support your body's healing. Make sure you’re drinking plenty of water.
If you’ve had a general anaesthetic, you might feel a bit nauseous initially. Starting with light, easy-to-digest foods like toast, soup, or yoghurt is a great idea. As your appetite returns, a balanced diet full of vitamins and minerals will give your body the fuel it needs to mend itself.
Try to avoid too much alcohol, as it can be dehydrating and might not mix well with any painkillers you’re taking. Some pain relief can also cause constipation, so upping your intake of fibre-rich foods like fruit, vegetables, and whole grains can help keep things moving. A healthy diet is a simple but powerful tool for a smooth recovery.
At The Vesey, we are committed to providing clear, supportive information to guide you through every stage of your healthcare journey. If you have more questions or wish to discuss a procedure, please don't hesitate to reach out to our expert team. https://www.thevesey.co.uk

