.webp)
Having your tonsils and adenoids out—what doctors call an adenotonsillectomy—is one of the most common surgical procedures for children. It’s generally recommended when these tissues start causing more harm than good, creating persistent health problems like chronic infections or breathing difficulties. The decision is made when the issues they cause far outweigh their normal job as part of the immune system.

Think of the tonsils and adenoids as the immune system's bouncers, stationed at the main entrances to the body. Located at the back of the throat and high up behind the nose, their job is to catch germs like bacteria and viruses that we breathe in or swallow. They essentially 'sample' these invaders, helping the body learn how to build its defences.
But sometimes, these gatekeepers become the problem. Instead of fighting off germs, they either get repeatedly infected themselves or grow so large they block the airways, interfering with normal life. When that happens, their protective benefits are completely overshadowed by the health issues they're creating.
There are really two main scenarios where these helpful tissues turn into a liability: chronic infection and obstruction. Both can seriously impact a person's quality of life, especially for a child.
Recurrent Infections: This is the classic case of tonsillitis. The tonsils become a hotspot for infection, leading to frequent, severe sore throats. Instead of protecting the body, they end up harbouring bacteria and causing illness over and over again.
Obstructive Issues: When tonsils and adenoids get too big, they can physically block the airway. This often forces constant mouth-breathing because it's hard to breathe through the nose. More seriously, it can lead to obstructive sleep apnoea (OSA), where breathing actually stops and starts repeatedly during sleep.
It’s important to realise that removing tonsils and adenoids isn’t about taking out something useful. It’s about removing a source of chronic illness or a dangerous obstruction to massively improve a person's overall health and wellbeing.
You can easily see the tonsils—they're the two round lumps of tissue at the very back of your throat. The adenoids, on the other hand, are hidden from view without special instruments. They sit much higher up, just behind the soft palate where your nasal cavity meets your throat.
Because they're so close to each other, a problem with one often involves the other. That’s why a combined removal of tonsils and adenoids is so common. For expert guidance on these conditions, you can learn more about professional ENT surgery options from specialists who can give you a detailed assessment and explain why this procedure might be the best solution for ongoing health concerns.

The decision to remove a child’s tonsils and adenoids is never taken lightly. An Ear, Nose, and Throat (ENT) specialist will only recommend surgery when these tissues are causing more harm than good—creating significant, persistent health issues that have a real impact on daily life.
The recommendation usually comes down to two main problems: relentless, recurring infections, or a physical blockage that dangerously gets in the way of breathing.
Think of it like a faulty security alarm. An alarm is there to protect you, but it becomes a massive liability if it’s constantly blaring for no reason (like recurrent infections) or physically blocking your doorway (like an obstruction). At that point, the most sensible thing to do is remove the faulty system to restore some peace and quiet.
One of the most common reasons for surgery is chronic tonsillitis. This isn't just about getting a sore throat a couple of times a year. We're talking about a miserable, relentless cycle of severe infections that cause missed school days, repeated courses of antibiotics, and a great deal of discomfort.
Before recommending surgery, an ENT specialist will look for a very clear pattern of illness. While guidelines can vary, a common threshold in the UK involves looking at a combination of factors:
The goal isn't just to stop sore throats. It's to break a debilitating cycle of illness that medication is no longer managing effectively.
Making this call involves a careful and thorough assessment. Clinicians often use established guidelines to inform their choices, and modern tools like Clinical Decision Support systems can help ensure recommendations align with best practices based on a patient's history. The first step is always a full evaluation, and understanding what happens during an ear, nose, and throat (ENT) assessment can help you feel prepared for that initial consultation.
The other major reason for removing tonsils and adenoids is when they simply get too big and physically block the airway. This can lead to issues like a constant nasal-sounding voice or habitual mouth breathing, but its most serious consequence is Obstructive Sleep Apnoea (OSA).
OSA is a condition where breathing literally stops and starts repeatedly during sleep. In children, the number one cause is enlarged tonsils and adenoids. The overgrown tissue acts like a plug at the back of the throat, closing off the airway when the muscles relax during sleep. This is a world away from simple snoring.
Key signs of OSA that parents should look out for include:
This is a critical health concern. In the UK, a huge number of tonsil and adenoid removals are performed for these obstructive reasons. One study highlighted that 83% of primary diagnoses for certain tonsillectomies were for obstruction, not infection.
It's also very common for both tissues to be removed together in a procedure known as an adenotonsillectomy. Research shows that around 91% of patients having their tonsils removed for obstruction also had their adenoids taken out at the same time, tackling the whole problem in one go.

The thought of any surgery can be nerve-wracking, but knowing exactly what to expect on the day can make all the difference. The process for tonsil and adenoid removal is a well-practised routine, designed to be as smooth and reassuring as possible for everyone involved.
From the moment you arrive at the hospital, our clinical team is there to guide you. It starts with pre-operative checks, where nurses will confirm a few details, take routine measurements like temperature, and answer any last-minute questions you might have.
You’ll also have a chat with the anaesthetist. They're the specialist doctor whose entire focus is on keeping the patient safely and comfortably asleep throughout the surgery. They'll explain how general anaesthesia works in simple terms and address any of your concerns. Understanding the comprehensive care involved in ear, nose, and throat surgery can bring a great deal of peace of mind.
Once the anaesthetic has taken effect and the patient is sound asleep, the operation begins. One of the most reassuring facts for many parents is that the entire procedure is performed through the mouth.
This means there are no external incisions, no cuts on the skin, and certainly no visible scars once everything has healed. The surgeon uses highly specialised instruments to work carefully at the back of the throat to remove the tonsil and adenoid tissue.
Modern surgical techniques have made a huge difference to the precision of this operation and how quickly patients recover. While traditional methods are still effective, many surgeons in the UK now use advanced tools to minimise discomfort and speed up healing.
Your surgeon will always discuss which technique is most suitable for you or your child, making sure you get the best possible outcome.
One of the biggest shifts in recent years is the move towards day-case surgery. For many patients, especially children, this means having the operation and heading home on the very same day. It's a fantastic approach that reduces disruption for the family and lets recovery happen in the comfort of your own home.
This isn't just a trend; it's backed by solid data. Over a decade, day-case tonsillectomies in the UK shot up from 33.2% to 59.2%. This change was made possible by advances like coblation becoming more common. Experts agree it streamlines the hospital experience and is more cost-effective for the health service, all without increasing the risk of complications.
A key factor for being eligible for day-case surgery is living reasonably close to the hospital with reliable transport. It’s a simple precaution that ensures you can get back for a check-up quickly if any concerns pop up.
The decision for day-case surgery is always made by the surgical and anaesthetic team. They'll look at a few key factors to make sure it's a completely safe option:
The team weighs up all these points to create a plan that is safe, effective, and right for each individual.
Getting through the recovery after a tonsil and adenoid removal is a huge part of the whole journey. Knowing what to expect day by day can turn what feels like a period of uncertainty into a clear, manageable healing process. Your main goal here is to stay comfortable, help the body heal, and keep an eye out for anything that might need a doctor's attention.
The whole thing is really a tale of two weeks, with different stages of healing. The first few days are all about managing pain, while the week after is about slowly getting back to normal eating and activities. Being organised and prepared is half the battle. For more on that, our guide on how to prepare for surgery has some great insights that can smooth out the process from the start.
This visual timeline gives you a bird's-eye view of the key recovery stages, showing you what to focus on and when.
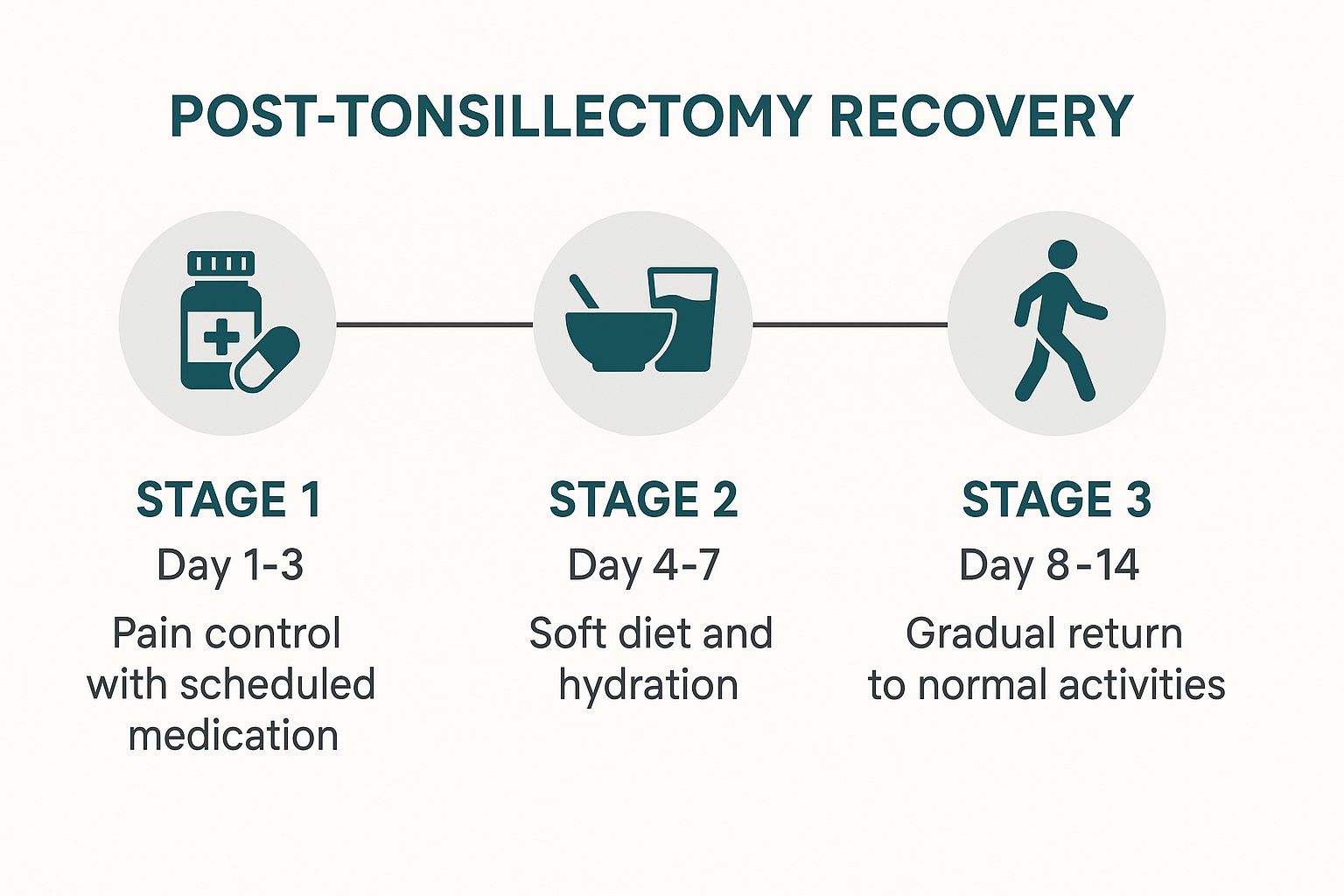
As you can see, recovery isn't random. It follows a pretty predictable path from immediate pain relief right through to getting back to normal life over about two weeks.
To give you a clearer day-by-day picture, here’s a breakdown of what you can typically expect during the post-surgery recovery period.
This table is a general guide, but remember that everyone heals at their own pace. Listening to your body (or your child's cues) is the most important thing.
Without a doubt, the first three days are the toughest. A very sore throat is the main event, so getting pain management right is your number one job.
The trick is to stay ahead of the pain. Don't wait until it’s unbearable before giving medication. Stick to the schedule your doctor prescribed—often alternating paracetamol and ibuprofen—to keep relief consistent. Setting alarms, even during the night, can be a lifesaver.
Key Insight: Consistent, scheduled pain relief is far more effective than trying to "catch up" once discomfort has set in. This proactive approach makes the first few days much more manageable for both children and adults.
From days four to seven, the sharpest pain usually starts to ease off, but the throat will still be incredibly tender. Hydration is absolutely crucial during this stage. You need to encourage constant sips of water, diluted juice, or ice lollies to keep the throat moist.
Now's the time to bust the myth that recovery is all about ice cream. While cold, soft foods feel great, a soft but relatively normal diet is actually encouraged to speed up healing. The simple act of swallowing helps to clean the area where the tonsils were and stops the throat muscles from getting stiff.
What to eat:
What to avoid:
A common and often surprising symptom this week is referred ear pain. This is a dull ache in the ears that's actually coming from the healing nerves in the throat. It's completely normal and usually responds well to regular pain relief.
Once you hit day eight, you should notice a massive improvement. The white or yellowish scabs that formed over the surgical sites will begin to fall away on their own. This is a good sign of healing, but it's also a time when there’s a slightly higher risk of bleeding.
Because of this, it's best to continue avoiding any strenuous activity for the full two weeks. That means no running, jumping, or heavy lifting. Most children should stay off school or nursery for up to 14 days to heal completely and avoid picking up any coughs or colds while their immune system is focused on recovery.
You can start a gradual return to a normal diet and activities during this second week. By the end of day fourteen, most people feel much more like themselves again. For more general advice on recuperation, this a practical guide to recovering from surgery at home offers some excellent tips that apply to all sorts of post-operative care.
Making the final call on tonsil and adenoid removal means looking carefully at both sides of the coin. Every surgical procedure has potential risks, and it's vital to understand them. But it’s just as important to weigh these against the significant, often life-changing, long-term benefits the operation can bring.
This balanced view is key to making a clear, informed choice. Think of it like deciding whether to fix a faulty foundation on your house. The repair work itself causes some disruption, but leaving it weak poses a much bigger, ongoing risk to the whole structure. You weigh the short-term inconvenience against long-term safety and stability.
The main risk everyone talks about with a tonsillectomy is bleeding after the operation. While it's uncommon, happening in only a small percentage of cases, it's the one your surgical team prepares you for most carefully. Knowing when and how it can happen is the best way to stay vigilant.
Bleeding is most likely to crop up during two specific windows:
Any sign of fresh, bright red blood from the mouth or nose is a signal to get medical help immediately. This could be spitting blood, vomiting blood, or, in a child, frequent swallowing – which can indicate blood is trickling down their throat. If you see any of these signs, you must go to the nearest A&E department straight away.
Other risks are much less common but still important to be aware of. These include an infection at the surgical site or a reaction to the general anaesthetic. Modern anaesthesia is incredibly safe, and your anaesthetist will have a detailed chat with you beforehand to minimise any potential issues. Protocols for enhancing surgical safety and reducing risks are a standard part of patient care, making sure every precaution is taken.
It's helpful to put these risks into context. Serious complications are rare. For the vast majority of patients, the procedure is straightforward and the recovery, while uncomfortable, is uneventful.
With the risks understood, let's turn to the powerful positive outcomes. For many families, the benefits of removing problematic tonsils and adenoids are profound and felt almost as soon as the two-week recovery period is over.
The improvements are often most dramatic in children who were suffering from Obstructive Sleep Apnoea (OSA). Once the airway is no longer blocked, the transformation can be remarkable.
For people plagued by chronic tonsillitis, the surgery offers a different but equally impactful kind of relief. It breaks a miserable cycle of frequent illness and reliance on antibiotics.
The benefits here are clear and direct:
Ultimately, the decision rests on a simple question: do the ongoing problems caused by the tonsils and adenoids outweigh the short-term risks of the surgery? For many, the answer is a clear yes, paving the way for a much healthier future.
Even after covering the basics, it's completely normal to have a few more questions rattling around. Deciding on a removal of tonsils and adenoids is a big step, and the key to feeling at ease is getting clear, straightforward answers.
Think of this section as our final chat, where we cover the practical, everyday concerns that pop up. My goal is to clear up any lingering uncertainties so you can feel confident and ready for what’s ahead.
This is, without a doubt, the number one concern for most parents. Since tonsils and adenoids are technically part of the immune system, is it safe to take them out? The answer, backed by decades of medical evidence and experience, is a firm yes.
While these tissues do catch germs, they’re only a tiny fraction of the body’s massive defence network. Study after study has shown that removing them doesn't weaken the immune system's long-term ability to fight off illness. The body has plenty of other resources to call upon, especially after the first few years of life when the immune system is fully developed.
In fact, for children with chronic tonsillitis, the tonsils have flipped from being defenders to being the source of the problem. Removing them actually boosts overall health by getting rid of a persistent infection hotspot.
Patience is everything when it comes to recovery. I strongly advise planning for a full two weeks at home before your child returns to school or nursery. Rushing back is one of the biggest mistakes we see.
This timeframe isn’t arbitrary; it serves two critical purposes:
All strenuous activities—sports, rough play, anything that gets the heart rate up—should also be off the table for the full 14 days. This is the best way to minimise the risk of bleeding. Your surgeon will give you specific advice, but two weeks is the solid guideline to plan your life around.
Knowing what to look for here is crucial. While significant bleeding is uncommon, it's the most serious potential complication, and spotting it early means you can act fast.
You must seek immediate medical help if you see any sign of fresh, bright red blood from the mouth or nose.
Here’s exactly what to watch for:
The risk is highest in two windows: the first 24 hours post-op, and again around days 7 to 10 when the protective scabs naturally start to come away. If you see any active bleeding, go straight to your nearest A&E for an urgent assessment. Don’t wait.
It's extremely unlikely the voice will change permanently for the worse. Any changes you notice are nearly always temporary or a clear improvement.
Right after the surgery, the voice might sound a bit different because of swelling in the throat. This is normal and usually settles down as the healing progresses over a couple of weeks.
For children whose very large tonsils and adenoids were causing a muffled, blocked, or nasal-sounding voice (we call this hyponasal speech), the surgery is often a game-changer. Once that obstruction is gone, the voice almost always becomes clearer and more natural than it was before. Any change is usually for the better.
At The Vesey, our dedicated ENT specialists provide exceptional care, guiding you through every step of the process with expertise and compassion. If you have further questions or wish to discuss whether the removal of tonsils and adenoids is the right choice for you or your child, we invite you to book a consultation with our team.