.webp)
A sudden, sharp stabbing pain in your knee is more than just an inconvenience; it's a clear signal from your body that something isn’t right. While it can be quite alarming, this sensation is often your body’s way of drawing a big red circle around a specific problem, which could be anything from a minor mechanical hiccup to a more significant joint issue.
Figuring out what’s causing it is the essential first step toward getting back on your feet, pain-free.

When you feel that sharp, stabbing sensation, it can stop you in your tracks. Think of it as your body's high-alert system—it's not a dull, generalised ache but a direct, pointed message that a specific part of your knee is in trouble. This kind of pain often points to an issue with one of the knee's more delicate structures, like the cartilage, ligaments, or the meniscus.
It’s a very different experience from a throbbing, constant ache. A stabbing pain is usually acute, appearing out of nowhere and often triggered by a particular movement—a twist, a deep bend, or even just putting weight on your leg. Making a mental note of exactly what you were doing when the pain hit can provide vital clues to its origin.
Getting to the bottom of what this sharp pain means is crucial. It’s typically associated with conditions that involve direct irritation or damage right inside the joint. Here are a few common culprits:
This guide will walk you through the most likely causes of your discomfort, from acute injuries to more chronic conditions. If you'd like a broader overview of joint problems, you can learn more about musculoskeletal pain and how we diagnose it.
A stabbing pain in the knee isn't just a symptom; it's a piece of diagnostic information. Its location, timing, and triggers help pinpoint the underlying cause, guiding you and your healthcare provider towards an effective treatment plan.
To get started, the table below gives a quick snapshot of common causes. Think of it as a starting point to help you connect your symptoms to a potential source before we dive into the details.
This table is just a starting point, of course. A proper diagnosis always requires a full assessment, but it can help you start to make sense of what your knee is trying to tell you.
That sudden, stabbing pain in your knee can be alarming. One minute you’re walking fine, the next you’re stopped in your tracks by a sharp, intense sensation. To get to the bottom of it, we need to look at what’s happening inside the knee joint itself. The causes generally fall into one of two camps: mechanical problems or inflammatory conditions.
Think of mechanical issues like a problem with a machine's moving parts—physical damage from an injury or simple wear and tear. Inflammatory conditions, on the other hand, are more like an internal system malfunction, where the body’s own processes create pain and swelling. Figuring out which category your pain fits into is the first step towards getting a clear diagnosis.
The infographic below gives a great visual overview of the most common culprits behind that stabbing feeling.
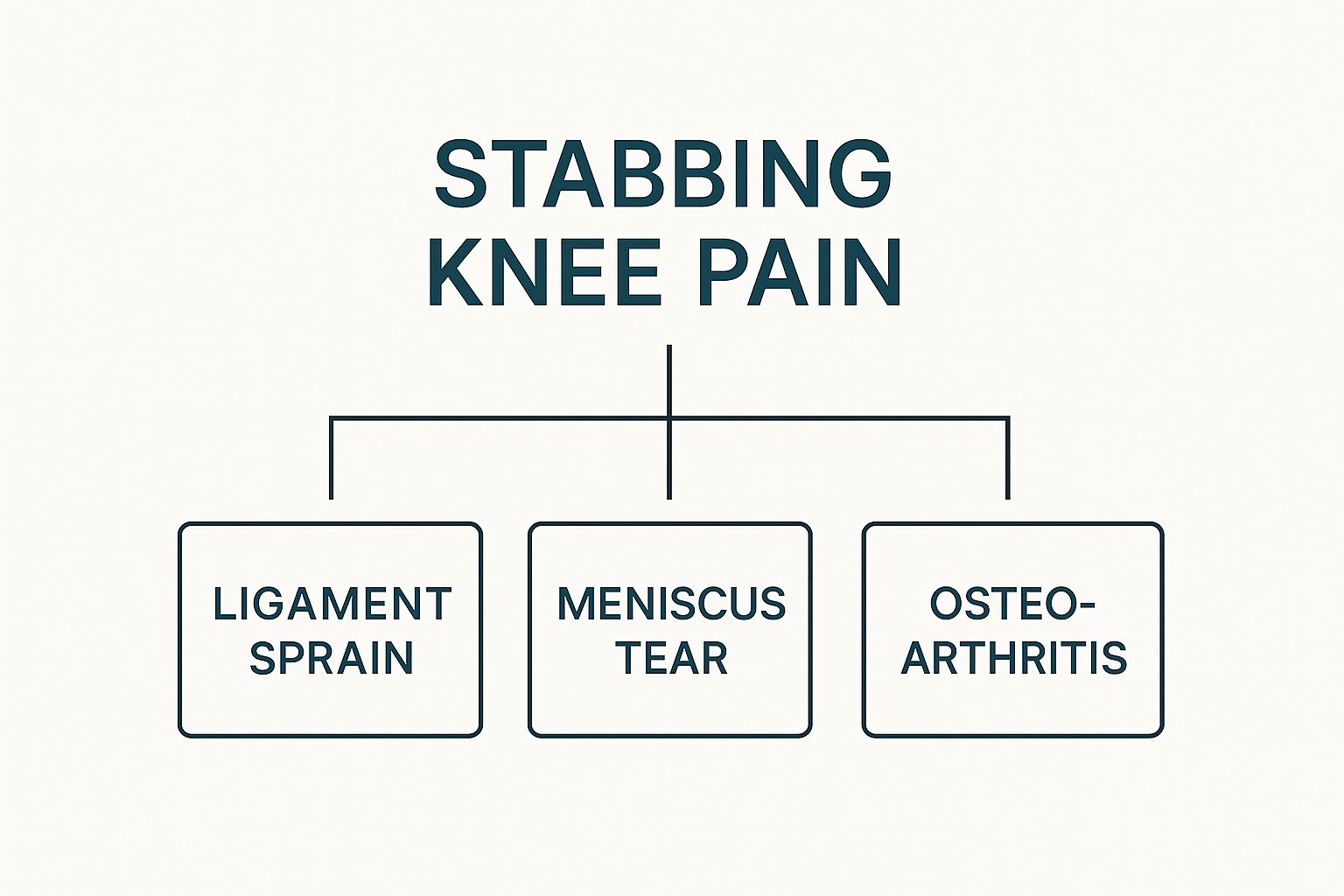
As you can see, a single symptom—stabbing pain—can point to very different issues within the knee, from torn soft tissue to worn-out cartilage.
When a mechanical fault is to blame, it’s usually because a specific part of the knee's structure has been torn, trapped, or damaged. These injuries are often acute, happening in a single moment, but they can also build up from repetitive strain over time.
A torn meniscus is one of the most common mechanical causes. The meniscus is a tough, C-shaped piece of cartilage that acts as a shock absorber between your shinbone and thighbone. If this tears, the loose flap can get caught in the joint as you move, causing a sharp, immediate pain and sometimes a feeling that your knee is locking up. This is a classic injury in sports that involve forceful twisting or deep squatting.
Another frequent offender is a ligament sprain or tear. Your knee has four main ligaments—think of them as strong, fibrous ropes holding everything stable. A sudden pivot, an awkward landing, or a direct hit can stretch or snap one of these ligaments, like the well-known Anterior Cruciate Ligament (ACL). The moment it happens, people often report hearing a "pop" followed by intense, stabbing pain deep inside the knee.
Unlike a sudden tear, inflammatory conditions often creep up more gradually, but they can still cause a sharp, stabbing pain. These problems start when the body’s natural response to damage or disease goes into overdrive, leading to swelling, redness, and pain inside the joint.
Osteoarthritis is a perfect example. This is the "wear-and-tear" type of arthritis, where the smooth, protective cartilage on the ends of your bones gradually wears down. While it’s often linked to a constant, dull ache, it can definitely cause stabbing pain. This happens when rough bone surfaces rub against each other or when small bone spurs (osteophytes) irritate nearby tissues during movement.
Knee pain is a massive issue in the UK, affecting roughly 25% of adults and seriously limiting mobility. Its prevalence has shot up by nearly 65% in the last two decades, a rise linked to obesity and an ageing population—both key risk factors for osteoarthritis. You can read the full study about the rising prevalence of knee pain and its risk factors.
Bursitis is another inflammatory culprit. Bursae are tiny, fluid-filled sacs that cushion the bones, tendons, and muscles around your joints. If a bursa in your knee gets irritated from repetitive pressure (like kneeling), it can become inflamed. This creates a sharp, localised pain that feels worse when you press on it or move the knee.
Finally, conditions like patellar tendinitis (often called "jumper's knee") involve inflammation of the tendon connecting your kneecap to your shinbone. This causes a sharp pain right below the kneecap, especially when you’re running, jumping, or climbing stairs. If you’d like to learn more, our guide on the symptoms and treatment of tendonitis goes into more detail.
By understanding these different causes, you can start to connect your specific symptoms—where the pain is, what movements trigger it, and any other sensations like clicking or instability—to a potential source. This is powerful knowledge to have when you speak to your doctor, helping you get one step closer to the right diagnosis and an effective plan to fix it.

Most of the time, stabbing knee pain can be managed with rest and a sensible visit to your GP. But some situations are much more serious, and knowing the difference between a niggle that can wait and a true emergency is crucial for your long-term joint health.
A simple way to think about it is like a traffic light. A green light is minor pain you can handle at home. A yellow light means it's time to book a doctor's appointment. But red light symptoms are a clear signal to stop everything and get immediate medical help. These could point to a severe injury or a dangerous infection that needs urgent care right now.
If you experience any of the following signs alongside that sharp, stabbing pain, it’s time to seek medical help straight away. These aren't "wait and see" symptoms. They’re clear warnings that something is seriously wrong inside the joint, and ignoring them could lead to permanent damage.
Here are the critical red flags:
An infected joint is a true orthopaedic emergency. Bacteria can cause irreversible damage to the cartilage in just a few days, leading to chronic pain and long-term disability if not treated immediately with antibiotics and drainage.
In a stressful moment, it can be tough to decide where to go—A&E or an urgent care centre. As a general rule, a severe deformity, uncontrollable pain, or signs of a serious infection absolutely warrant a trip to the emergency room.
For issues that are still urgent but less severe, understanding the difference between services can save you time and get you the right help. You can find more details in our guide on choosing between the emergency room vs urgent care.
Recognising these red flags gives you the confidence to act fast. When it comes to a potential emergency, seeking prompt medical advice isn't an overreaction; it's the most important step you can take to protect your knee.
Walking into a clinic with a sharp, stabbing pain in your knee can be unsettling. But the diagnostic process isn’t guesswork; it’s more like a detective gathering clues to solve a case, starting with the most important evidence—your own experience.
The journey begins with a detailed chat and a hands-on physical exam. Your doctor will want to know the story behind your pain: what it feels like, when it started, and what makes it better or worse. This conversation is invaluable, as the little details often point straight to the likely culprit.
Following the discussion, your doctor will perform a physical examination. This is far more than a quick look; it's a careful, methodical assessment of your knee’s structure and function.
The physical exam is a hands-on investigation to check your knee's stability, range of motion, and overall health. Your doctor will likely ask you to lie down, sit, and stand, observing how your knee behaves in different positions. They’ll also gently press on various parts of the joint to pinpoint the exact source of that stabbing pain.
This stage often involves a few specialised manoeuvres to test specific parts of your knee. For example, your doctor might perform:
This examination helps your doctor form an initial idea of what’s going on, which then guides the decision on whether more advanced tests are needed to get the full picture.
A thorough physical examination is often the most revealing part of the whole process. How your knee responds to specific movements and pressures provides direct evidence of what’s happening inside the joint—often before any imaging is even considered.
If the physical exam isn’t conclusive or suggests a more serious issue, your doctor will turn to imaging tests. Think of these as different types of cameras, each designed to capture a specific kind of detail inside your knee.
An X-ray is usually the first port of call. It’s like taking a black-and-white photograph of your bones and is fantastic for spotting things like:
But an X-ray has its limits—it can’t see soft tissues like ligaments, tendons, or cartilage. If your doctor suspects damage to these structures, they'll order a more detailed scan.
A Magnetic Resonance Imaging (MRI) scan provides an incredibly detailed, 3D map of your entire knee joint, showing both bone and soft tissue. An MRI is the gold standard for diagnosing issues like a torn meniscus, a ligament tear (like an ACL injury), or cartilage damage. It uses powerful magnets and radio waves to create cross-sectional images, allowing the doctor to see the exact location and severity of an injury.
In some cases, a Computerised Tomography (CT) scan might be used. A CT scan combines a series of X-rays taken from different angles to create a more detailed view of the bones than a standard X-ray. It’s particularly useful for assessing complex fractures. If you’re curious about the process, you can read our guide on how long a CT scan typically takes.
Sometimes, that stabbing pain is centred around the front of the knee. Patellofemoral pain syndrome (PFPS) is a very common culprit, especially among active people in the UK. One systematic review revealed its annual prevalence is around 22.7% in the general population, climbing to 28.9% in adolescents. You can discover more insights about patellofemoral pain and its prevalence to understand this common condition better.

Once your doctor has pinpointed the cause of that sharp, stabbing pain, the focus immediately shifts to finding a solution. The best treatment plans usually start with simple, effective strategies you can manage at home before exploring more advanced medical interventions. It's about building a recovery roadmap that doesn't just silence the immediate pain but also promotes long-term joint health.
This foundational approach is key. By managing acute symptoms like swelling and pain right away, you create a much better environment for your knee to start the healing process. From there, your plan can be scaled up as needed, with professional guidance to get you back on your feet safely and for good.
For immediate relief after a new injury or a sudden flare-up, the P.R.I.C.E. method is an incredibly effective first-aid protocol. It's a simple, memorable acronym that walks you through the five essential steps to manage acute knee pain and inflammation.
Think of it as your emergency toolkit for joint injuries. Each letter represents a step with a specific job, and together, they work to minimise damage, control swelling, and kick-start the healing process.
The P.R.I.C.E. method is more than just a set of instructions; it’s a strategy to control the body’s initial inflammatory response. By managing swelling and pain early, you create a much better foundation for the deeper healing that needs to follow.
While at-home care is vital, many causes of stabbing knee pain need a professional eye to achieve a full recovery. Your doctor will tailor a treatment plan based on your specific diagnosis, how severe it is, and what your lifestyle goals are.
A cornerstone of professional care is almost always physiotherapy. A skilled physiotherapist will design a targeted exercise programme to rebuild strength in the muscles that support your knee, like the quadriceps and hamstrings. This doesn't just help you recover; it builds resilience against future injuries.
For those interested in natural approaches, it's worth exploring the potential of castor oil for joint pain relief, which many people find helpful for easing pain and reducing inflammation.
When conservative treatments aren't cutting it, your doctor may suggest more direct interventions. These are designed to target the source of the inflammation or damage right inside the joint itself.
Medications are often used to manage symptoms. Over-the-counter non-steroidal anti-inflammatory drugs (NSAIDs) can be very effective for bringing down both pain and swelling. For more severe cases, your doctor might prescribe stronger options.
Injections can deliver powerful relief directly where it's needed most.
In the UK, knee osteoarthritis is a major driver of stabbing knee pain, affecting an estimated 5.4 million people. The condition has a significant impact, with over 30 million prescriptions for musculoskeletal issues costing the NHS around £139 million in 2022-2023.
For severe structural damage, such as a complete ligament tear or advanced arthritis that hasn't responded to anything else, surgical options may be the next step. These can range from minimally invasive arthroscopic surgery to repair a torn meniscus, all the way to a full knee replacement for end-stage arthritis. Your surgeon will discuss the best route to restore function and finally eliminate your pain.
Getting over that initial stabbing pain in your knee is the first major victory, but the real goal is keeping it from coming back. To do that, we need to shift from reactive treatment to proactive care. It’s all about building a natural support system for your joints so they can handle whatever life throws at them.
Think of the muscles around your knee as its own personal team of bodyguards. When these muscles are strong, they absorb most of the impact and strain that would otherwise go straight to the joint. But if they're weak, your knee is left vulnerable to every little shock and twist, massively increasing the risk of another injury.
The most important players on your knee's support team are the quadriceps (front of your thigh), hamstrings (back of your thigh), and glutes (your bum). Strengthening these three groups creates a powerful, stabilising framework around the entire joint. A consistent routine of targeted, low-impact exercises can make a world of difference.
You don't need anything complicated. Start with these foundational movements:
One thing is non-negotiable: proper form. Doing exercises incorrectly can do more harm than good, creating new imbalances or straining the very joint you’re trying to protect. If you’re not sure, working with a physiotherapist to get the technique right is a brilliant investment. To really build resilience, it's also crucial to understand how to prevent common running injuries, including knee pain.
Building knee resilience isn't about pushing through pain; it's about smart, consistent strengthening. Each repetition of a controlled exercise is like adding another layer of armour around your joint, making it far less susceptible to future damage.
Beyond specific exercises, a few lifestyle changes play a massive role in protecting your knees. First up, maintaining a healthy weight is one of the most impactful things you can do. Every extra pound of body weight adds four to six pounds of pressure onto your knee joints. That means even a modest weight loss provides substantial relief.
Choosing your activities wisely is also key. High-impact sports like running on hard surfaces can be really jarring for the knees. Instead, consider swapping in some knee-friendly alternatives like swimming, cycling, or using an elliptical machine. These give you a fantastic cardiovascular workout and build muscle without the repetitive pounding that can aggravate a sensitive joint.
By combining targeted strengthening with mindful lifestyle choices, you're creating a solid blueprint for stronger, more durable knees that can carry you forward, pain-free.
Even after getting to grips with the causes and treatments, you’ll likely still have a few practical questions about handling that sharp, stabbing pain in your knee. Getting straight answers to these everyday worries is a huge part of managing your recovery and feeling more in control.
Here, we tackle some of the most common questions we hear, offering straightforward advice to help you navigate the day-to-day reality of knee pain.
Yes, absolutely. While a sudden fall or awkward twist is a common culprit, that stabbing pain often comes from conditions that have been building up for a while. Overuse issues like patellar tendinitis or degenerative diseases such as osteoarthritis are perfect examples.
In these situations, the pain doesn't come from a single traumatic event. Instead, it’s the result of chronic inflammation or the slow, steady wearing down of cartilage. It means you can feel a sudden, sharp pain during a normal movement without any obvious injury to blame.
Finding a comfortable sleeping position is crucial when your knee is screaming at you. It gives the joint a chance to rest and recover properly.
To take the stress off your knee, try sleeping on your back with a pillow propped underneath both knees. This gives them just enough support to keep the joint in a relaxed, neutral position.
If you’re a side sleeper, place a pillow between your knees. It’s a simple trick, but it works wonders by aligning your hips and pelvis, stopping your top leg from twisting downwards and straining your sore knee overnight.
This is a classic question, and the answer depends on what’s causing the pain. A good rule of thumb is: ice for injury, heat for ache.
For a new injury or a sudden flare-up with swelling (usually within the first 48 hours), grab an ice pack. Apply it for 15-20 minutes at a time. The cold helps constrict blood vessels, which reduces inflammation and numbs that sharp pain. On the other hand, for chronic stiffness or a dull ache without swelling—like from arthritis—a heating pad is your friend. The warmth helps relax tight muscles and boosts circulation to the area.
Your body is the best judge here—listen to what it’s telling you. If the pain is severe or you feel like your knee might give way, stop immediately and rest. Pushing through intense pain is a recipe for making the underlying problem much worse.
If the pain is milder, some gentle walking might be okay. But if that stabbing feeling sticks around or gets worse with every step, that's your cue to stop. It’s always best to get a proper diagnosis before you continue with any activity that’s causing you discomfort.
At The Vesey, our specialists are dedicated to diagnosing the source of your knee pain and creating a personalised treatment plan to get you back to your life. For exceptional care across all medical specialties, visit us at https://www.thevesey.co.uk.

