.webp)
A women's health check-up is far more than just a routine appointment. It’s a dedicated time for proactive, preventative care, where you can have an open conversation with a healthcare professional about your overall wellbeing. Many know it as a "well-woman exam," but it’s best to think of it as an ongoing dialogue to safeguard your future health.

It’s all too easy to see a doctor's appointment as just another task on a never-ending to-do list, especially when you're juggling work, family, and everything in between. But it's time to reframe that thinking. This check-up isn't a chore or simply a hunt for problems; it’s a moment you set aside to prioritise yourself. It’s a powerful act of self-care and a conscious investment in your long-term health.
This is your time with a GP or practice nurse—a safe space to discuss anything that's on your mind, from menstrual cycle worries to your mental health, without feeling rushed. It's about empowering you to take charge of your health with confidence.
Preventative care is really the heart of a women's health check-up. Think of your health like a car. You don't wait for the engine to seize up on the motorway before you take it to the garage. You schedule regular services to keep it running smoothly and catch any small issues before they turn into major, expensive repairs.
Routine health screenings work in exactly the same way. They’re designed to spot potential problems long before you'd ever notice symptoms. This early detection is absolutely critical for conditions like cervical or breast cancer, where treatment is most successful when it’s started as early as possible.
A preventative check-up is your chance to team up with a healthcare professional and create a personalised roadmap to keep you healthy for years to come. It’s about being proactive, not reactive.
Every check-up you have adds another layer to your personal health story, creating a vital baseline. When your doctor has a clear record of what's "normal" for you—your typical blood pressure, weight, and cholesterol levels—they can spot any significant changes that might be a red flag for an underlying issue.
This ongoing record isn't just a collection of numbers; it helps build a complete picture. It's about understanding the trends and patterns unique to your body. Part of this proactive self-care means getting to know specific health risks, like familiarising yourself with the signs of heart problems unique to women. This kind of knowledge allows you and your doctor to make better-informed decisions together, tailoring advice and screenings to what truly matters for your wellbeing.
Just as your life shifts and changes with every passing decade, so do your health needs. What’s a priority for a woman in her 20s looks quite different from her concerns in her 50s. Understanding this natural evolution is the key to making your women's health check up a powerful tool for lifelong wellbeing.
This isn’t about a generic, one-size-fits-all checklist. Think of it instead as a personalised health roadmap, one that adjusts to your age, lifestyle, and unique risk factors. Let's walk through the key screenings and health conversations you should be having at every stage of your life.
These decades are truly foundational for your health. The habits you build now can echo for years to come, making this the perfect time to establish a strong, trusting relationship with your GP and really get to know your personal health baseline.
The most significant screening during this period is the cervical screening, better known as a smear test. In the UK, you'll get your first invitation around your 25th birthday. This simple test checks for high-risk types of human papillomavirus (HPV), which can cause changes to the cells of your cervix.
Despite how important it is, attendance isn't always what it should be. Cervical screening is offered to women in England aged 25 to 64, yet recent NHS data revealed that of the 5.12 million women invited for screening, only 68.8% attended. That’s a huge number of women missing a crucial chance for early detection and prevention of cervical cancer—a disease the NHS aims to eliminate by 2040.
Beyond cervical screening, your 20s and 30s are an ideal time to:
As you step into your 40s, your body starts undergoing subtle but important changes. This is when preventative care begins to focus more on conditions that become more common with age, and when conversations about your long-term health really come to the forefront.
For many women, this decade marks the start of perimenopause—the transitional period just before menopause. The symptoms can be incredibly varied and sometimes confusing, so tracking any changes you notice can be really helpful for your GP.
Key health considerations for this decade include:
Your 40s are all about proactive monitoring. By keeping a close eye on key health markers like blood pressure and cholesterol, you are taking powerful steps to protect your future health and wellbeing.
Your 50s represent a significant milestone in women's health. It’s when the NHS breast screening programme begins, with invitations sent every three years to women aged between 50 and 71. This screening uses a mammogram, an X-ray of the breast, to find early signs of cancer when it's most treatable.
This is also the decade when most women experience menopause. The transition can bring a whole host of physical and emotional symptoms, from hot flushes and sleep problems to changes in mood. It's so important to have an open conversation with your GP, as there is a great deal of support available. You can also learn more about managing menopause and perimenopause in our detailed guide.
From your 50s onwards, the focus of your health check-up broadens:
The following table summarises some of the most common screenings and when they are typically recommended in the UK.
This visual guide breaks down the journey quite nicely.
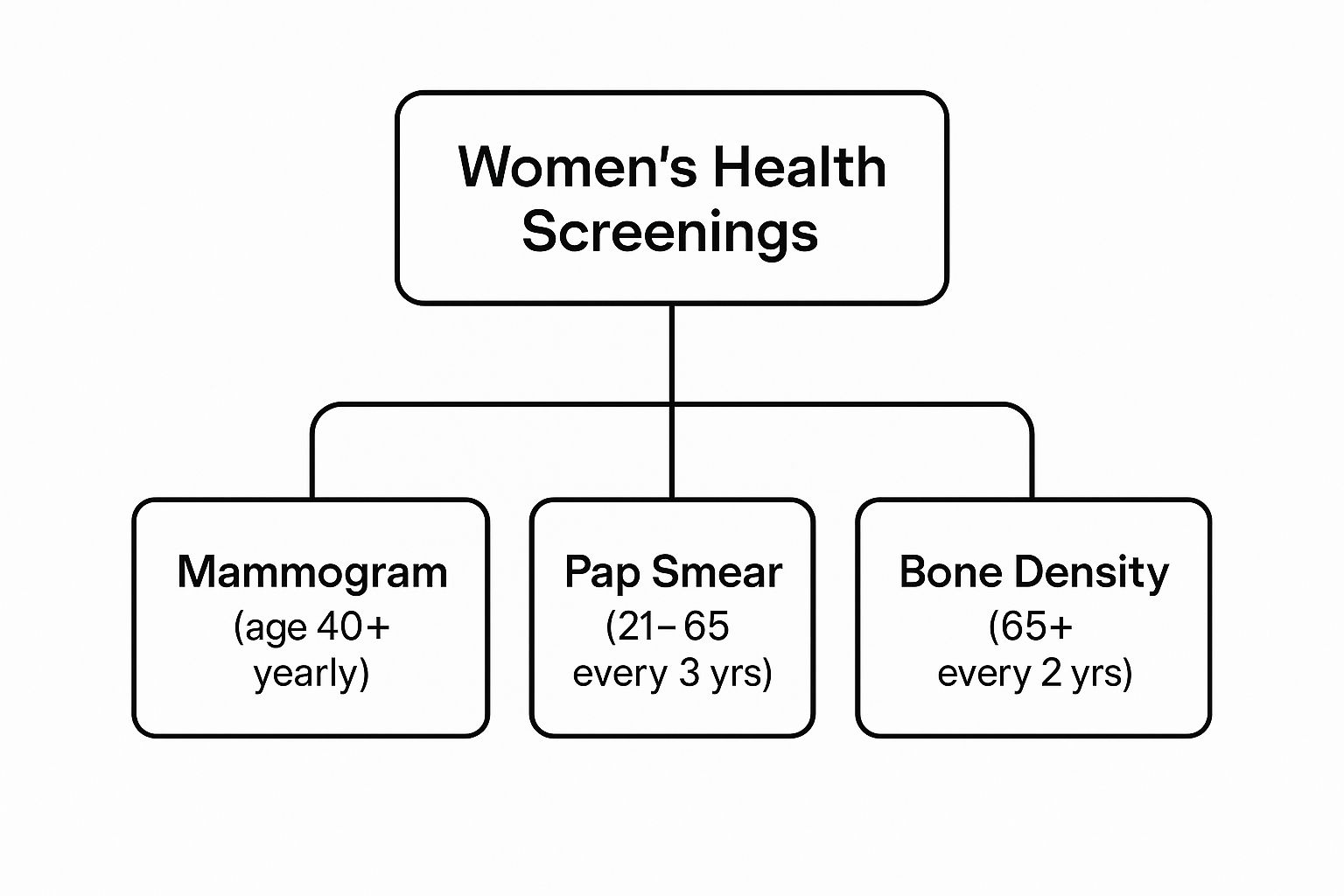
It clearly illustrates how the focus shifts from reproductive health in our younger years towards cancer and bone health monitoring as we get older.
Remember, your health journey is entirely unique. This decade-by-decade guide is just a framework, not a rigid set of rules. The most important step you can take is to maintain an open dialogue with your healthcare provider, ensuring your care is always aligned with your current life stage and personal needs.

For many women, the cervical screening—or smear test, as it's often called—is the most familiar part of a women's health check-up. It's also one that can be surrounded by a fair bit of anxiety and confusion. Let's cut through the noise and give you a straightforward, reassuring guide to what it's all about, so you can feel empowered by knowledge, not worried.
First things first, it's vital to know what the test is actually looking for. It isn’t a test for cancer. In the UK, modern cervical screening is designed to test for high-risk types of the human papillomavirus (HPV). HPV is an incredibly common virus that most of us will encounter at some point, and in the vast majority of cases, our bodies simply clear it without any trouble.
However, certain high-risk strains of HPV can, over a long time, cause changes to the cells in the cervix. If left unchecked, these changes could eventually lead to cancer. Think of the screening as a preventative early warning system: it finds high-risk HPV infections first, which allows for close monitoring or early treatment of any cell changes, long before they become a serious problem.
Knowing what happens step-by-step can make the whole experience feel much less intimidating. The test itself is very quick, usually taking less than five minutes. You’ll be shown to a private space to undress from the waist down and given a sheet to cover yourself with.
The nurse or doctor will ask you to lie on an examination couch. They then gently insert a smooth, tube-shaped tool called a speculum into your vagina, which allows them to get a clear view of your cervix.
Using a tiny, soft brush, they’ll quickly sweep a small sample of cells from the surface of your cervix. It might feel a bit unusual, but it shouldn't be painful. As soon as the sample is taken, the speculum is removed, and that's it—you're done. You can get dressed and go about your day.
The most important thing to remember is that you are in complete control. You can ask the nurse to stop at any time or to explain what they are doing. They are there to make you feel as comfortable as possible.
A few weeks after your appointment, you’ll receive a letter with your results. The terminology can be a bit confusing, so let’s break down what the different outcomes really mean.
The UK's screening programme has evolved significantly, with the UK National Screening Committee now recommending this HPV test every five years for women aged 25 to 64. Despite the programme's incredible success, attendance has sadly dropped, with about a third of invited women not taking part. To help make this life-saving check more accessible, self-sampling kits are being trialled for women who are overdue for screening.
If you have any questions or feel particularly anxious, please chat with the practice nurse beforehand. For more information on the process, you can also check out our dedicated cervical screening information page.

Standard screening guidelines are a fantastic starting point for your health, but they’re designed for the average person. The reality is, your body and your life are unique, which means your women's health check up plan should be too. Truly effective preventative care isn't a one-size-fits-all checklist; it's a strategy built specifically for you.
Think of the standard advice as the basic framework of a house. It’s solid and reliable, but it only becomes a home when you add your own personal touches—the colours, the furniture, the little details that reflect who you are. Personalising your health plan works the same way; it’s about layering your individual risk factors onto that strong foundation.
This is a partnership between you and your doctor. By sharing a complete picture of your health, family history, and lifestyle, you can work together to create a check-up schedule that perfectly matches your personal needs, making sure nothing important gets overlooked.
Your family’s medical history is one of the most powerful tools for personalising your health plan. It’s like a genetic road map, highlighting potential health conditions you might be more susceptible to. It’s absolutely vital to know about and discuss any significant health issues that have affected your immediate family.
This doesn't mean you’re destined to develop the same conditions, but it does signal to your GP that earlier or more frequent screenings might be a good idea. It’s all about being vigilant and proactive.
Key conditions to be aware of in your family history include:
Beyond your genes, your daily habits and lifestyle choices play a huge part in your overall health profile. Being completely open with your doctor about your lifestyle allows them to recommend specific tests or offer tailored advice that addresses your unique circumstances.
For instance, if you’re a smoker, your GP will have a very different conversation with you about lung health and cardiovascular risk compared to a non-smoker. Your diet also has a massive influence. As part of tailoring your health plan, understanding your nutritional needs is key. You might find it helpful to learn about calculating your daily calorie needs to better support your wellness goals.
Your health plan should be a living document, not a rigid script. It should adapt not only to your age but also to your family history and the life you lead every day.
By having these honest conversations, you shift from being a passive recipient of healthcare to an active partner in your own wellbeing. You empower yourself and your GP to build a truly preventative strategy, ensuring your women's health check-up is as effective and relevant as it can possibly be. This personalised approach is the key to protecting your health for the long run.
Knowing you need a women's health check up is one thing, but actually getting yourself to the appointment is another story entirely. Life gets incredibly busy, and it's all too easy to let your own health slip down the priority list. Beyond the simple challenge of finding the time, many of us also grapple with emotional hurdles like anxiety or embarrassment.
Feeling a bit nervous about a check-up is completely normal, especially if you know it involves an intimate examination like a smear test. It's crucial to remember that healthcare professionals do this every single day. Their goal is to support you and make you feel as comfortable as possible. These barriers are real, but they are absolutely beatable.
Often, the biggest hurdle is simply a fear of the unknown, or feeling self-conscious. For procedures like cervical screenings, these feelings can be a major roadblock. A 2025 survey highlighted this, showing that 16% of eligible UK women have avoided smear tests altogether. The number climbs even higher to 20% among Generation Z, often due to fear and misconceptions about the test. You can read more about smear test attendance on axahealth.co.uk.
To help put your mind at ease, remember you have options. You can always:
Remember, you are in control of your appointment. Your comfort is a priority, and healthcare staff are trained to support you through any nervousness you may feel.
A little bit of prep work can completely change the dynamic of your appointment, turning it from a source of stress into an empowering and productive chat. Getting organised beforehand ensures all your concerns are addressed and you get the most out of your time with the doctor or nurse. Think of it as a mini-project dedicated to your wellbeing.
Here’s a simple checklist to get you ready:
Taking these steps means you’ll walk in ready for a proper discussion, making the entire visit far more effective. For anyone wanting a more comprehensive assessment, exploring a private well person check could offer a deeper dive into your health.
Even with a world of information at our fingertips, it's completely normal to still have questions about your health. Medical advice can often feel a bit complicated, but getting clear, simple answers is the best way to feel confident and in control of your own wellbeing.
This section is all about answering some of the most common practical questions women in the UK have about their health check-ups. We’ll demystify the process, explain the difference between NHS and private options, and hopefully offer some reassurance for any worries you might have.
One of the biggest points of confusion is how to actually book a 'well-woman' check. The truth is, in the UK, it isn’t a single, specific appointment you can book on the NHS. Instead, preventative care is handled through a series of targeted national screening programmes and your routine GP consultations.
For scheduled screenings like your smear test, you don't need to do a thing to get the ball rolling. You'll automatically get an invitation letter from the NHS when you're due. Once that letter lands on your doormat, you just need to call your GP surgery to book in with the practice nurse.
For anything else, like checking your blood pressure, discussing contraception, or talking about your mental health, you'd book a standard appointment with your GP. It’s also handy to know that many local pharmacies now offer free blood pressure checks without an appointment.
The main difference between NHS and private health checks really comes down to scope, frequency, and cost. The two systems are designed to do different things, and understanding this can help you decide what’s right for you.
The NHS provides essential, evidence-based screenings free of charge to everyone. These are carefully aimed at specific age groups where they’ll have the biggest impact on preventing major diseases.
The trade-off, of course, is the cost. While a private check gives you a deeper look, it does come with a significant price tag. For anyone interested in this route, you can learn more about how private healthcare works in the UK and what your options might be.
Feeling anxious about a cervical screening is incredibly common, so please know you are not alone. The most important thing to remember is that you are in control, and the nursing staff are there to help you feel as comfortable as possible.
Being open is your best tool. Let the nurse know you're feeling nervous right from the start. They are highly experienced in supporting anxious patients and can change their approach to help you feel more at ease.
It is completely your right to ask the nurse to slow down or stop at any point during the procedure. Your comfort and consent are the top priorities.
Here are a few practical things you can request or do that might make the experience a bit easier:
The test itself is very quick, usually lasting just a few minutes. A moment of potential discomfort provides years of reassurance and vital protection for your health.
Getting a letter saying your results are 'abnormal' can be a really frightening moment. But it's so important to understand that this word rarely means you have cancer. It just means some changes have been found that need a closer look.
The whole point of screening is to find these early changes when they are easiest to manage.
Your GP or the screening unit will always explain what the results mean and what comes next. An abnormal result means the system is working exactly as it should—by catching potential issues at the earliest possible stage.

