.webp)
Facing the thought of surgery for an ovarian cyst can feel overwhelming. The first step, though, is simply to understand why it might even be on the table.
Most ovarian cysts are completely benign. Many don’t cause any symptoms at all and often disappear on their own without anyone needing to do a thing. But when certain signs pop up, the conversation can shift from simple observation to actively treating it, and that's when ovarian cyst removal comes into play.
The path from finding an ovarian cyst to discussing surgery isn’t always a straight line. Think of most cysts as temporary bubbles; they appear and then quietly resolve on their own over a few menstrual cycles.
Because of this, the most common first step is what we call "watchful waiting." It’s exactly what it sounds like: we monitor the cyst with follow-up ultrasounds to see if it changes size or, ideally, goes away by itself.
But this hands-off approach isn’t right for every situation. Your gynaecologist will suggest moving towards surgery based on a few clear indicators. It's rarely one single thing, but more of a big-picture view of what the cyst is doing and how it’s affecting you.
Several factors can quickly change the conversation from "let's wait and see" to "let's get it removed." These are the main things we look for in the UK when recommending surgery:
A woman’s age and whether she's gone through menopause play a huge part in how we approach a cyst. The game plan is quite different because the risk profile changes significantly after menopause.
In the UK, while the overwhelming majority of ovarian cysts in premenopausal women are harmless, the risk of a cyst being cancerous is higher for women over 50. UK guidelines push for careful observation in many cases, but surgery is usually the recommended path for cysts that are large, causing symptoms, or look suspicious on a scan.
This balanced approach ensures we only operate when it's truly necessary. We avoid intervening with harmless cysts but act decisively when there are clear signs of a potential problem.
Understanding these factors helps take the mystery out of why ovarian cyst removal might be recommended, putting you in a much better position to chat through all the options with your doctor.
If surgery ends up being the best way forward, knowing what’s involved can make the whole process feel less daunting. The type of surgery your specialist recommends will depend on a few things: the size and type of the cyst, and whether there’s any concern it might be cancerous.
You can think of it like needing to fix something inside a locked box. You could either use tiny, precise tools through small keyholes, or you could open the entire lid to get a clear, direct view. In surgery, these two methods are known as laparoscopy and laparotomy.
This infographic gives a quick overview of how doctors decide between monitoring a cyst ('watchful waiting') and moving forward with surgery.
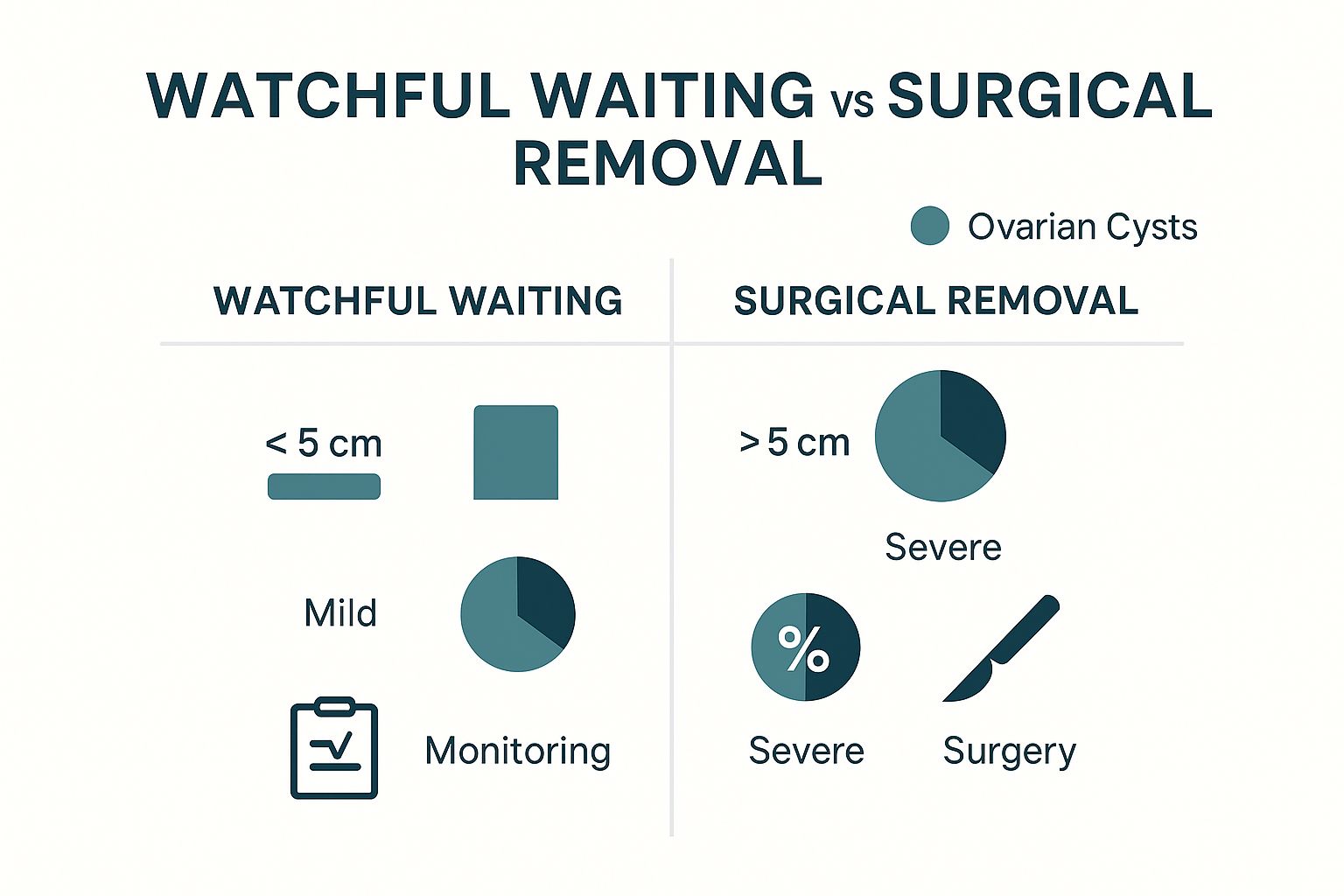
As you can see, smaller cysts with mild symptoms are often just monitored for a while. It’s the larger, more troublesome ones that usually lead to a recommendation for surgery.
Laparoscopic surgery is the most common method for ovarian cyst removal in the UK. This minimally invasive technique is the go-to for a reason: it means less pain and a much faster recovery.
Imagine a mechanic using specialised tools and a tiny camera to work on an engine without having to lift the entire bonnet. That’s pretty much what happens during a laparoscopy. The surgeon makes a few small cuts in the abdomen, often around the belly button.
Through these little openings, they insert a laparoscope—a thin tube with a light and a camera—along with other surgical instruments. Your abdomen is gently inflated with carbon dioxide gas to create some space, giving the surgeon a clear view of your ovaries on a screen. From there, they can carefully remove the cyst.
In the UK, keyhole surgery is the standard of care for most benign cysts. The benefits are significant, with most women being treated as day cases or requiring just a single overnight stay in hospital. You can learn more about the patient experience with gynaecological keyhole surgery to better understand the process.
This approach causes minimal scarring and disruption to the surrounding tissues, which is why getting back on your feet is so much quicker.
A laparotomy, or open surgery, is the more traditional route. It’s reserved for specific situations, like when a cyst is particularly large, if there's a strong suspicion of cancer, or if there’s a lot of complex work to be done.
Instead of small keyholes, the surgeon makes a single, larger incision across the abdomen—a bit like the cut for a caesarean section. This gives them direct, unobstructed access to the pelvic organs, allowing them to safely remove a very large or complex mass.
While it’s a more invasive procedure with a longer recovery time and a more noticeable scar, sometimes it is simply the safest and most effective option.
To make the differences clear, here’s a straightforward comparison between the two main surgical methods.
Ultimately, the choice between laparoscopy and laparotomy isn't about one being "better" than the other. It's about which one is the safest and most effective tool for your specific situation.
Beyond how the surgery is done, there’s the crucial question of what exactly is removed. The goal is always to be as conservative as possible, especially for women who may want to have children in the future.
There are two main outcomes:
UK clinicians carefully tailor the surgical approach to each patient's unique situation, balancing the need for effective treatment with long-term health and fertility goals. This patient-centred planning ensures you receive the most appropriate and effective care possible.
Feeling in control before an operation can make a huge difference. Knowing you’ve done everything to prepare doesn't just calm the nerves; it helps set you up for a much smoother recovery.
Think of the weeks leading up to your surgery as your preparation time. It’s not just about the medical side of things, but also about getting your home and support network ready. By sorting things out beforehand, you can put all your energy into what matters most afterwards: resting and healing.
Before your surgery date is confirmed, you'll come in for a pre-operative assessment. This is a crucial check-up to make sure you're fit and ready for both the anaesthetic and the operation itself. We'll go through your medical history, any medications you're currently taking, and run a few routine tests.
This assessment usually includes:
This is the perfect time to ask any last-minute questions about the ovarian cyst removal itself. Seriously, no question is too small or silly, so please ask whatever is on your mind.
Your surgeon will give you a specific set of instructions to follow. It’s incredibly important to stick to these, as they are designed for your safety and to ensure the best outcome.
Medication Adjustments
You might be asked to temporarily stop taking certain medicines, like blood thinners or even some herbal supplements. This is usually done a few days before your operation to minimise any risk of bleeding. Make sure your surgical team has a complete list of everything you take.
Fasting Instructions
You will be given a strict time to stop eating and drinking before the procedure. This is a standard safety protocol to make sure your stomach is empty before you have a general anaesthetic.
Following these instructions to the letter is non-negotiable. Sticking to the fasting and medication guidelines is one of the most important things you can do to help us keep you safe.
What happens after you leave the hospital is just as important as the surgery itself. A little planning now can make your return home so much less stressful. Try batch-cooking a few simple meals and popping them in the freezer – you’ll be glad you did when you don't feel up to standing at the stove.
Set up your space for easy living. Keep things you use often—like the remote, your phone charger, and a water bottle—within easy reach of your main resting spot. It’s also a great idea to line up a friend or family member to help with chores or just to check in on you for the first couple of days. For more detailed advice, have a look at our complete guide on how to prepare for surgery.
Packing a small, well-thought-out bag will make your stay much more comfortable. Even if you're only in for a short time, which is common for keyhole surgery, having a few home comforts can make all the difference.
Essential Hospital Bag Checklist:

Trying to understand the path through the NHS for something like ovarian cyst removal can feel a bit overwhelming, but getting to grips with the typical steps can help you feel more in control. It all usually starts with a visit to your GP. If they suspect an ovarian cyst needs a closer look, they’ll refer you to a specialist.
This referral is your first step into secondary care, where you’ll be seen by a gynaecology team. It’s here that they’ll organise more detailed tests, like specialised ultrasounds, to get a much clearer picture of what’s going on. Based on those results, they’ll decide on a plan—which could be monitoring the cyst or moving forward with surgery.
Once your GP makes that referral, you're officially on a waiting list to see a gynaecologist. How long you wait for this first appointment can vary quite a bit, depending on where you live and how busy your local NHS trust is at the time.
When you see the gynaecologist, they'll go over your symptoms, your medical history, and any scans you’ve already had. They might also do a physical examination before discussing their findings with you in detail. This is your chance to really understand what kind of cyst you have and why surgery might be on the table.
As you navigate the healthcare system, you'll come across a lot of medical jargon. Getting a handle on certain concepts, like understanding medical diagnostic codes like ICD-10, can make it easier to follow your medical records and communications.
It’s really important to have a realistic view of waiting times within the NHS. Gynaecological services are under immense pressure right now, which has a direct knock-on effect on how long you might wait for a diagnosis and, ultimately, for treatment like ovarian cyst removal.
Recent figures paint a stark picture: the gynaecology waiting list has ballooned to over 750,000 women, more than double what it was before the pandemic. A huge number of these women are waiting longer than the 18-week target set by the NHS, and the backlog is especially bad for surgical procedures.
The urgency of your case is the biggest factor in how quickly you get seen. Cysts that are very large, causing severe pain, or have features that look suspicious will always be prioritised. Even so, priority cases for ovarian cyst removal can face long waits because of staff shortages and a lack of available operating theatre time.
This can be incredibly frustrating, and for some, it leads them to consider other routes. If you're weighing up your options, you might find our guide on what private healthcare involves helpful.
Waiting is often the hardest part, but you don't have to be passive. There are things you can do to stay informed and feel more in control. For starters, don’t be afraid to contact the gynaecologist's secretary to ask for an update on your position on the list.
It's also vital to keep your GP in the loop about any changes to your symptoms. If your pain gets worse or you start experiencing new, worrying symptoms, let your GP know straight away. They can pass this information on to the hospital, which might change the urgency of your case.
Here are a few key questions you can ask your healthcare team to stay informed:
Asking these questions puts you back in the driver's seat. Navigating the system takes patience, but staying engaged can help manage your expectations and ease some of the anxiety that comes with the wait.

Recovering from an ovarian cyst removal is very much a journey, not a race. The single most important thing you can do is give your body the time and space it needs to heal properly. Your recovery path will look a little different depending on the type of surgery you had, but knowing the general milestones helps you feel prepared and patient with your body’s progress.
Think of it as a gentle climb back to your full strength. The first few days are always the steepest part, but things get gradually easier week by week. The key is to listen to your body and not push yourself too hard, too soon.
Straight after your operation, you’ll be moved to a recovery room where the nursing team will keep a close eye on you as you come around from the anaesthetic. It’s completely normal to feel groggy, a bit disoriented, and maybe even a little nauseous.
Pain is also expected, but the team will be right there to make sure you have medication to keep it well under control. You might also notice some odd discomfort in your shoulders if you had keyhole surgery. This is a very common and temporary side effect from the gas used to inflate your abdomen, and it will pass.
Once you’re discharged and settled at home, your main job is to rest. This is especially true during that first week. You’ll likely feel more tired than usual, and that’s because your body is putting a huge amount of energy into healing itself.
It is absolutely essential to avoid any heavy lifting. This means no carrying heavy shopping bags, laundry baskets, or even small children for several weeks. Straining your abdominal muscles too early can seriously interfere with how your internal and external wounds heal.
As you head into the second week and beyond, you’ll slowly start to feel more like yourself again. But the timeline for getting back to your normal routine really depends on whether you had keyhole or open surgery. The recovery from a hysteroscopy, for example, has its own unique timeline, which can be useful as a comparison. For more on that, you can read about the typical hysteroscopy recovery time in our other guide.
For ovarian cyst removal, healing is always a gradual process.
After Laparoscopy (Keyhole Surgery):
Most women feel significantly better within one to two weeks. You can usually get back to a desk job and other light activities around this time. Driving is typically okay once you can perform an emergency stop without any pain, which for many is also around the two-week mark.
After Laparotomy (Open Surgery):
This is a longer road. Recovery usually takes between four to six weeks, and sometimes even longer. You’ll need to plan for more time off work and will have much stricter limits on physical activity. It can take a few months to feel fully back to strength.
This table gives a general idea of what to expect, but remember it’s just a guide.
These are just estimates, and it’s crucial to follow the specific advice of your surgeon. Your personal recovery timeline will always depend on your individual health and the exact details of your procedure.

Knowing what to expect is half the battle. When you’re considering an ovarian cyst removal, a clear, balanced view of the potential risks and the long-term picture is absolutely vital. It empowers you to have a confident conversation with your surgeon and helps you feel prepared for every part of the journey.
Like any surgery, removing an ovarian cyst comes with a standard set of risks. Modern medicine has made these complications rare, but it’s still important to be aware of them.
These are the same potential issues you’d face with most abdominal operations:
Beyond the general surgical risks, there are a couple of points specific to ovarian surgery. One is the small possibility of damage to nearby organs, like the bladder or bowel. Surgeons are incredibly skilled at navigating these delicate areas, but it remains a known, if infrequent, complication.
Another big question we often hear is, "Can the cyst come back?" Unfortunately, yes, a recurrence is possible. Cyst development is often tied to hormonal fluctuations, especially oestrogen. This means that even after a successful removal, new cysts can sometimes form on the same ovary or the other one. Regular follow-up appointments are key to monitoring for any new developments.
Having a complete picture of your health is crucial for both medical decisions and personal planning. As you think about the long-term impact of surgery, it's natural to also consider how your medical history might affect other areas of life, like looking into life insurance for pre-existing medical conditions.
For many women, the number one concern is how an ovarian cyst removal will affect their future fertility and overall health. The great news is that the long-term outlook is generally very positive, and it all comes down to the extent of the surgery.
Impact on Fertility:
Your surgeon’s goal will always be to preserve as much healthy ovarian tissue as possible. Understanding these potential outcomes helps you discuss your family planning goals and make the best decision for your future.
Going into any kind of surgery can feel overwhelming, and it’s completely normal to have questions. Let’s clear up some of the most common concerns we hear from patients about ovarian cyst removal.
It’s possible, yes. Many cysts are tied to your natural hormonal cycle, especially oestrogen. So, even after a successful removal, your body can still form new ones down the line.
This isn’t a sign the surgery failed—it’s just how ovaries work. That’s why regular check-ups are so important for keeping an eye on your long-term ovarian health.
This is a huge concern for many women, and understandably so. The good news is that the answer depends on the type of surgery, and preserving fertility is always a top priority.
Your surgeon’s goal is always to preserve as much healthy ovarian tissue as possible, putting your future fertility first whenever it is safe to do so.
A common myth is that removing one ovary halves your chances of getting pregnant. In reality, the other ovary usually steps up to compensate, allowing for normal fertility. It’s a key point to talk through with your specialist.
Absolutely. For many small, harmless cysts that aren’t causing any symptoms, the best first step is often "watchful waiting."
This simply means we monitor the cyst with follow-up ultrasound scans over a few months to see if it disappears on its own—which many do. We usually only recommend surgery when a cyst is very large, causing persistent pain, or looks suspicious.
Your recovery time really depends on which surgical method is used.
At The Vesey, we believe in providing clear, compassionate, and expert care from your first consultation to your final check-up. If you have more questions or would like to discuss your options with a specialist, please get in touch by visiting https://www.thevesey.co.uk.