.webp)
If you're pregnant for the first time, the NHS typically schedules around 10 antenatal appointments. If this isn't your first baby, it's usually closer to 7. These visits kick off with a 'booking appointment' around 8-10 weeks and then continue with key scans and check-ups, becoming more frequent as you get closer to your due date.
Feeling a bit overwhelmed by the journey ahead is completely normal, but having a clear roadmap of what's to come can make everything feel much more manageable. Think of this as your personal pregnancy calendar, designed to help you prepare for each conversation with your midwife, from that first booking visit right through to the final checks before birth.
The whole point is to give you the knowledge you need to feel confident and play an active part in your own antenatal care. When you understand the purpose of each visit, you know exactly what to expect and what questions you might want to ask. It can also be helpful to understand how clinics manage their diaries, often using a patient access scheduler to keep things running smoothly.
Your care is structured around a series of crucial check-ins and scans that keep a close eye on both your health and your baby's development. Getting to these appointments, especially early on, is vital for the best possible outcomes.
The timeline below highlights the three most important early milestones in your antenatal appointment schedule.
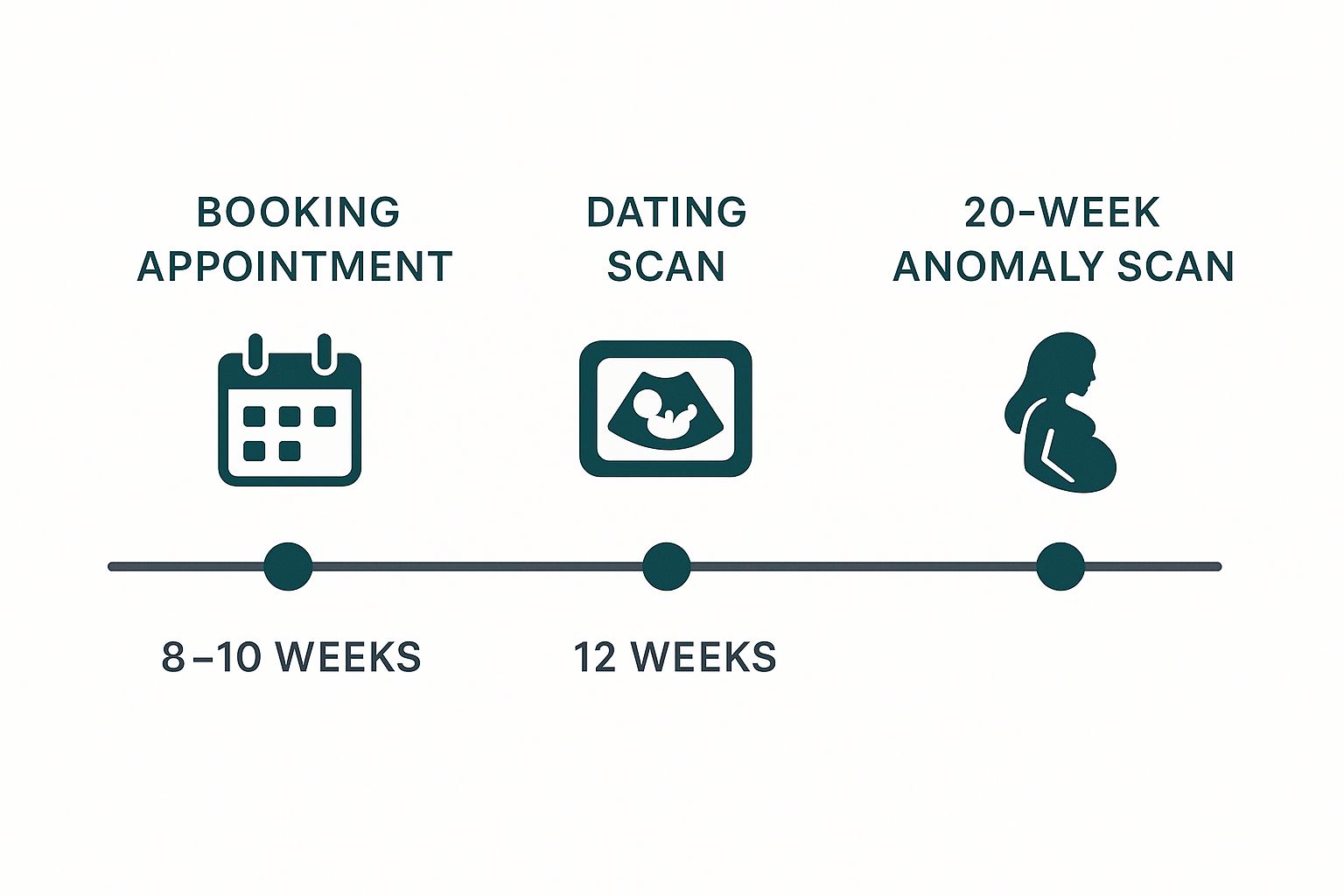
As you can see, your care starts early, with that initial booking appointment laying the groundwork for all the monitoring and scans that follow.
However, data shows that timely access isn't always straightforward. Across England, just over 60% of pregnant women have their first booking appointment by the recommended 10-week mark, and these rates can vary quite a bit depending on region and ethnicity. If you need to get your first visit in the diary, you can easily book appointments online at The Vesey.

The first trimester is all about setting a strong foundation for the months ahead. Your first few appointments are crucial for confirming your pregnancy, assessing your health, and putting a plan in place for a healthy journey.
It used to be that your first stop was always the GP, but things have thankfully become more direct. NHS England has rolled out a digital self-referral portal, meaning you can book your first midwife appointment yourself without needing to see a doctor first. This simple change has made a huge difference – nearly 60,000 women used it shortly after it launched, getting them into the system faster. You can read more about how the NHS is improving midwife appointments here.
That all-important first meeting with your midwife is called the "booking appointment," and it usually takes place between weeks 8 and 10. This is a really comprehensive session where your midwife gets a full picture of you, your health history, and anything specific to your pregnancy.
Think of it as a detailed MOT for your pregnancy. Your midwife will chat with you about your medical background, your partner's health, and any previous pregnancies. This helps them build a complete picture so they can give you the best possible care. A key part of this is understanding your overall reproductive health.
During this visit, you'll also have a few routine checks:
Your midwife is your main point of contact and support. Never be afraid to ask questions, no matter how small they feel. This is the perfect time to talk about any worries, get tips for managing morning sickness, or just get a clear idea of what’s coming next.
Around the 12-week mark, you'll get an invitation for your first ultrasound, often called the dating scan. For most parents-to-be, this is an incredibly exciting moment – the first proper glimpse of their baby.
But this scan is about more than just a lovely picture for the fridge. Its main job is to accurately work out your estimated due date (EDD) by measuring your baby from head to bottom.
The sonographer will also check:
At this appointment, you'll also be offered a combined screening test for Down's, Edwards', and Patau's syndromes. This involves a blood test alongside a nuchal translucency (NT) measurement taken from the scan. This screening is entirely optional, and your midwife will give you all the information you need to decide what’s right for you.

As you sail into the second trimester, covering weeks 13 to 27, you might notice your prenatal appointment schedule feels a bit more relaxed. The initial flurry of activity gives way to a new focus: monitoring your baby's steady growth and checking in on your own wellbeing. You’ll typically see your midwife around week 16 and again at week 25.
These appointments are reassuring checkpoints. Your midwife will continue with the familiar, yet vital, checks of your blood pressure and urine. These simple, consistent measurements are crucial for spotting early signs of conditions like pre-eclampsia and help build a valuable picture of your health over time.
A new measurement also makes its debut during this trimester: the symphysis-fundal height (SFH). It sounds complex, but it's a straightforward check where your midwife uses a tape measure to track the distance from your pubic bone to the top of your womb. Starting from around week 24, this simple measurement gives a fantastic indication of your baby’s growth rate.
The main event of the second trimester is, without a doubt, the detailed ultrasound that happens between 18 and 21 weeks. It’s often called the anomaly scan, and it’s a much deeper dive than your first scan.
A highly trained sonographer will carefully examine your baby from head to tiny toe. They’ll be looking at the development of the major organs like the heart and brain, checking the position of your placenta, and measuring the amount of amniotic fluid. It's an incredible opportunity to see just how much your little one has grown.
The purpose of the anomaly scan is to check for a range of conditions and to ensure your baby is developing as expected. While the vast majority of scans show no issues, it provides an important opportunity to identify any concerns early.
The scan screens for 11 specific physical conditions, including issues related to the spine, abdominal wall, and kidneys. And yes, if you want to find out the sex, this is usually the time you can! Just be sure to let the sonographer know your preference beforehand.
Here's a quick look at the key scans and screening tests you can expect during the second trimester.
These tests provide a comprehensive picture of both your and your baby's health as you move through this middle stage of pregnancy.
Your midwife appointments are also the perfect time to chat about how you're feeling. Many women find this trimester brings a welcome energy boost, but it's still so important to discuss any symptoms or worries you might have. You may also be offered further blood tests to check for things like anaemia. Understanding the different blood testing procedures can be very helpful and takes a lot of the mystery out of the process.
To get the most out of your visits, try these simple tips:

You’ve made it to the final stretch! From week 28 until your baby arrives, the third trimester is all about exciting anticipation and final preparations. You’ll notice your prenatal care appointments become much more frequent now, which is a sure sign you’re getting very close to the big day.
Typically, you can expect to see your midwife every two weeks from week 30 to 36. After that, it’s weekly until your baby is born. This ramped-up schedule allows your care team to keep a close eye on your health and your baby’s positioning as you approach your due date.
During these last appointments, your midwife will continue the routine checks of your blood pressure, urine, and the symphysis-fundal height to make sure your baby is growing well. A major focus now shifts to figuring out your baby’s position. Your midwife will gently feel your abdomen to check if the baby has settled into the best head-down position for birth.
Another important check happens around week 28, with a repeat blood test for anaemia. It’s quite common for iron levels to dip in late pregnancy, and this test ensures you have the energy stores you’ll need for labour and recovery. If you are Rh-negative, you'll also be offered an anti-D injection around this time to protect your baby.
These visits are also the perfect opportunity to have in-depth conversations about the birth itself. Now is the time to finalise your birth plan and talk through your preferences in detail.
Your midwife will guide you through all the available pain relief options, from gas and air to epidurals, helping you understand the pros and cons of each. This is your chance to ask every question you have, ensuring you feel empowered and informed about the choices ahead.
As your due date gets closer, the conversations will naturally turn towards recognising the first signs of labour. Your midwife will walk you through what to look for—things like contractions starting or your waters breaking—and explain exactly when you should call the hospital or midwifery unit. Talking through these practical steps can really help ease any anxiety and make you feel much more prepared.
This is also the time to get all your ducks in a row. As you run through the final preparations with your midwife, don’t forget to pack your bags. A good hospital bag checklist will make sure you have everything you need. Deciding where you want to give birth is another huge decision, and understanding your options at the best maternity hospitals in your area can bring real peace of mind.
From week 37, your pregnancy is officially considered "full-term." Your weekly appointments will continue to monitor the baby's position and wellbeing. From week 40 or 41, your midwife may offer a "membrane sweep" to help encourage labour to start naturally. These final checks are all about making sure you and your baby are safe, healthy, and ready for a smooth delivery.
Think of the standard prenatal appointment schedule as a brilliant road map—but remember, not every journey follows the exact same route. It’s completely normal for your schedule to be personalised based on your health and your baby’s needs, making sure you both get the right level of support.
If your midwife or doctor recommends a more tailored plan with extra appointments or scans, it isn’t a cause for alarm. It’s simply a sign of proactive, individualised care designed to keep you both as safe and healthy as possible.
Your care team might suggest more frequent visits if certain health factors are part of your story. This just allows them to keep a closer eye on things and step in early if any issues start to bubble up.
Common reasons for extra monitoring include:
This shift to a more frequent or specialised schedule is known as consultant-led care. It means an obstetrician (a doctor specialising in pregnancy and birth) will have overall responsibility for your care, working alongside your midwifery team.
So what does a change in your prenatal schedule actually look like? It usually means more regular check-ups and potentially more detailed scans.
For instance, if your baby is in a breech position late in pregnancy, you might have extra appointments to discuss your options, like an External Cephalic Version (ECV) or planning for a caesarean birth.
If you’re managing something like high blood pressure, you might be asked to come in more often for blood pressure checks and urine tests. These extra visits are all about prevention—spotting and managing any changes right away.
Sadly, not everyone has equal access to consistent antenatal care. Research highlights that maternal mortality rates in the UK are significantly higher for women from more deprived areas and for Black women. A key issue identified in these findings is the barrier some women face in simply getting to their appointments. You can read the full MBRRACE-UK report for more insights on maternal health disparities.
This really underscores how vital it is to have a flexible and supportive care system that adapts to every individual’s circumstances, ensuring everyone gets the monitoring and support they need.
Navigating your prenatal care can feel like you’re learning a whole new language, full of appointments, scans, and unfamiliar terminology. It’s completely natural to have a long list of questions along the way. Getting clear, straightforward answers is the key to feeling confident and in control of your pregnancy journey.
We’ve put together some answers to the most common queries we hear from expectant parents. Think of this as your go-to guide for demystifying the practical side of your appointment schedule.
Life happens, and sometimes you just can't make an appointment. The moment you know you need to reschedule, give your midwife or the maternity unit a call directly. They really do understand that things come up and will help you find a new slot that works.
This is especially important for time-sensitive visits like the 12-week dating scan or the 20-week anomaly scan. These scans have to be done within a specific window to get accurate results, so it's crucial to rearrange them as quickly as possible. If you can, giving at least 24 hours’ notice is always appreciated, as it helps the clinic manage their schedule for everyone.
Yes, absolutely. In most cases, you’re welcome and even encouraged to bring your partner or another trusted support person with you. Their presence can be incredibly comforting, helps them feel more involved, and gives you an extra set of ears for all the important information being shared.
Having a support person at key appointments, especially the scans, can make the experience feel more special and less daunting. They can help you remember the questions you wanted to ask and recall the midwife's advice afterwards.
Just be aware that individual NHS trusts sometimes have specific policies, particularly for scan rooms where space might be limited or where they need to maintain a calm environment. It’s always a good idea to check your local hospital’s current guidelines online before you go.
A little bit of prep goes a long way in getting the most out of every single appointment. The best thing you can do is keep a running list of any questions or concerns that pop into your head between visits. A small notebook or a note on your phone works perfectly for this.
And, of course, always remember to bring your handheld maternity notes with you. This folder is essentially your pregnancy passport, holding all the vital information about your journey so far. Coming prepared with your questions and your notes ensures you won't forget anything important and helps you feel much more in control of your care. For more general advice and details, you can also find a wealth of helpful patient information covering a wide range of topics.
If you’ve gone past the recommended 10-week mark for your first booking appointment, please don’t panic. The key is to act quickly. Get in touch with your GP or local maternity services right away to get yourself booked in.
While getting started earlier is ideal for timing certain screening tests, the most important thing is simply to begin your antenatal care. The midwifery team will do everything they can to get you caught up on all the necessary checks and blood tests, making sure you and your baby are on the right track for a healthy, well-supported pregnancy. Just make that call as soon as you can.
At The Vesey, we are committed to providing exceptional, personalised care throughout your entire journey. Our expert teams are here to support you at every stage, ensuring you feel informed, comfortable, and confident. Explore our comprehensive services at https://www.thevesey.co.uk.