.webp)
Ever felt a bit breathless and wondered what’s really going on inside your lungs? A pulmonary function test (PFT) is designed to answer exactly that. It’s a series of straightforward, non-invasive breathing exercises that measure how well your lungs are performing.
Think of it as a comprehensive health check for your respiratory system. These tests give us hard data on everything from your lung volume and capacity to how quickly you can move air and how efficiently your body absorbs oxygen.
If your lungs were a car engine, a PFT would be the full diagnostic check. It goes far beyond simply seeing if the engine turns on; it measures its horsepower, fuel efficiency, and overall performance. In the same way, a PFT provides your doctor with precise, objective numbers about every aspect of your breathing.
It allows us to move past guesswork and get a clear, detailed picture of what’s happening. These tests are a cornerstone of modern respiratory medicine, helping specialists investigate unexplained symptoms and manage long-term conditions effectively. Your GP or a respiratory consultant might suggest a PFT for several key reasons.
One of the most common reasons for a pulmonary function test is to get to the bottom of persistent symptoms. If you're dealing with a nagging cough, wheezing, or shortness of breath, a PFT can help pinpoint the underlying cause.
To give you a better idea, here are some of the main scenarios where a PFT is invaluable.
As the table shows, PFTs are crucial for both diagnosis and ongoing management. For patients with a known condition, regular testing shows us whether the illness is stable or if we need to adjust the treatment plan. It can also be a vital safety check before surgery to ensure a patient is fit enough for anaesthesia.
Sometimes, respiratory symptoms can be influenced by your surroundings. It can be useful to investigate factors in your home environment; for instance, you might want to look into professional air quality testing services for your home's health.
A pulmonary function test provides critical, measurable insights into your lung health. It transforms subjective symptoms like "feeling breathless" into objective data that can guide an accurate diagnosis and effective treatment plan.
In the UK, where lung conditions are the third biggest killer, the importance of accurate diagnostics really can't be overstated. Tests like spirometry, a common PFT, are absolutely vital for managing widespread diseases like COPD and asthma.
Unfortunately, access isn't always equal, with some areas facing a 'postcode lottery' that can lead to delayed diagnoses and poorer outcomes. This reality underscores just how essential timely and accurate PFTs are for public health. By providing such detailed metrics, these tests empower healthcare professionals to intervene early and effectively, improving the quality of life for millions.
A pulmonary function test isn't a single, one-size-fits-all assessment. It’s actually a family of different tests, each designed to measure a specific aspect of your lung performance. Think of it like a mechanic’s diagnostic toolkit; you wouldn’t use a pressure gauge to check the electrics. In the same way, your doctor will select the right combination of tests to build a complete, detailed picture of your respiratory health.
These tests work together to answer a few crucial questions. How much air can your lungs actually hold? How quickly can you move that air in and out? And, most importantly, how well does oxygen get from your lungs into your bloodstream? Let's break down the main types you're likely to come across.

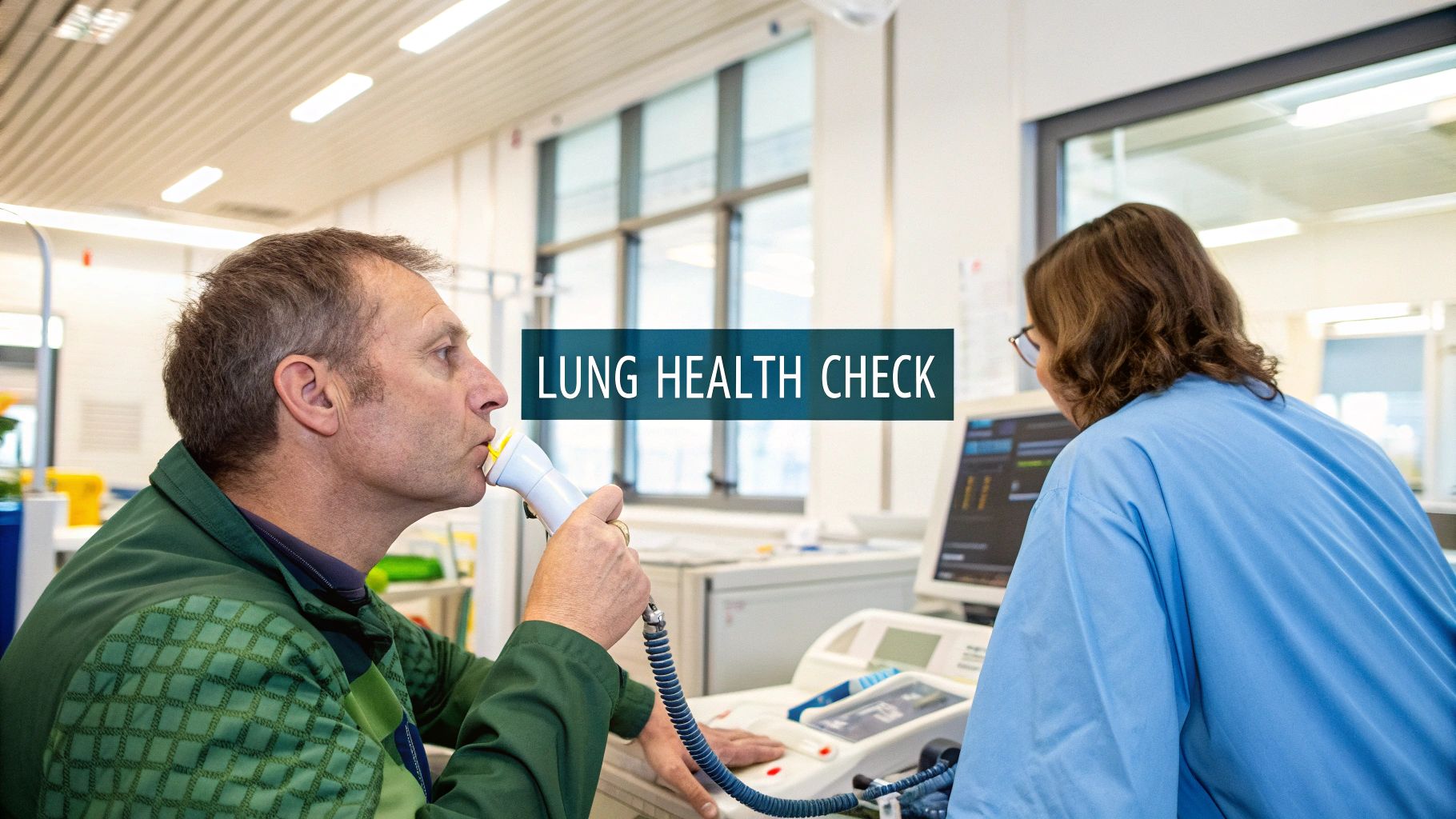
Spirometry is the most common and fundamental PFT out there. It’s the true workhorse of lung diagnostics, focused on measuring airflow—that is, both the volume of air you can breathe and the speed at which you can move it.
Imagine your lungs are a set of bellows. Spirometry is all about measuring how much air you can force out and how quickly you can do it. During the test, you’ll take a huge, deep breath and then exhale as hard and as fast as you possibly can into a mouthpiece, which is connected to a machine called a spirometer.
This test is particularly brilliant for spotting obstructive lung diseases, where something is physically hindering the airflow out of your lungs. Conditions like asthma or Chronic Obstructive Pulmonary Disease (COPD) often cause the airways to narrow, which a spirometry test can pick up with remarkable accuracy.
While spirometry is great for measuring airflow, it can’t tell us the total size of your lungs. For that, we need a lung volume measurement, often done using a technique called body plethysmography. This test is designed to determine your total lung capacity (TLC).
Think of this as finding out the maximum volume of a balloon, not just how fast you can let the air out. To do this, you sit inside a small, airtight, clear enclosure that looks a bit like an old-school phone box. You'll breathe into a mouthpiece while a sensor measures tiny pressure changes inside the box around you.
Those small pressure changes allow the technician to precisely calculate the total volume of air your lungs can hold. This is a key measurement for diagnosing restrictive lung diseases, where the lungs themselves are stiff or unable to expand fully, such as in pulmonary fibrosis.
A complete pulmonary function test often combines spirometry with lung volume and diffusion tests. This multi-faceted approach ensures doctors don't just see one part of the picture, but get a detailed, 360-degree view of your overall lung health.
Finally, we have the gas diffusion test (or DLCO test). This assesses how efficiently your lungs transfer oxygen from the air you breathe into your bloodstream. It’s the ultimate quality control check on your respiratory system's most important job.
The best analogy here is a coffee filter. It doesn’t matter how much water you pour in if the filter itself is clogged and can't let the good stuff through. This test measures how well the thin membranes in your lungs, called alveoli, are doing their job of exchanging gases.
During the test, you'll inhale a small, completely harmless amount of a tracer gas (like carbon monoxide). You’ll then hold your breath for about 10 seconds before exhaling. The machine analyses how much of that tracer gas you breathed out, which tells us how much was absorbed into your blood. This provides a direct measure of your lungs' diffusion capacity.
This test is vital for identifying damage to the lung tissue itself, often caused by conditions like emphysema or interstitial lung diseases. It's also a common component in many workplace health assessments, which is why some employers arrange for specialised evaluations. You can learn more about how these fit into a wider health context by exploring information on occupational medicals. By combining these different tests, your healthcare provider can assemble a detailed diagnostic puzzle, leading to a much more accurate diagnosis and a better-tailored treatment plan.
Right, let's get you ready for your pulmonary function test. A little bit of prep work beforehand can make all the difference, ensuring the results we get are a true reflection of your lung health. Think of it as clearing the decks – we want to remove anything that could temporarily throw off the numbers.
Thankfully, it’s all very straightforward. We’re just looking to get a clean baseline measurement of how your lungs perform on a normal day, without any interference from things like tight clothes, a big meal, or recent exercise.
On the day of your test, a few simple adjustments will help us get the most accurate readings possible.
These small steps ensure we’re measuring your lungs’ typical performance, not how they’re reacting to immediate physical stress.
This is probably the most important part of your preparation, especially if you use inhalers.
Your doctor absolutely needs to know which medications you’re taking, as some can have a direct impact on the test. It’s quite common to be asked to hold off on certain inhalers, particularly bronchodilators – the ones that work by opening up your airways.
Crucial Note: Never stop taking any medication unless your doctor has specifically told you to. They will give you clear instructions on exactly what to pause and for how long.
Why do we do this? Sometimes, the test is done twice: once at the start, and then again after you’ve used a bronchodilator. This lets us see if the medication helps open up your airways, which is a key piece of the puzzle for diagnosing conditions like asthma. Pausing your usual dose means we start from a true baseline.
Along with the points above, there are a few other things to steer clear of to ensure your results are spot-on.
By following these simple steps, you’re helping us gather the most accurate data about your lung health. That information is what allows your doctor to make a confident diagnosis and map out the most effective treatment plan for you.
Walking into an appointment for a pulmonary function test can feel a bit daunting if you don’t know what’s coming. The good news is that the whole process is straightforward, non-invasive, and you’ll be guided by a friendly professional from start to finish.
Let’s walk through what a typical appointment looks like so you can feel completely at ease.
From the moment you arrive, you’ll be in the capable hands of a respiratory physiologist or a clinical scientist. Their main job is to make you feel comfortable, clearly explain every step, and coach you through the breathing exercises to get the most accurate results possible.
Before the main tests kick off, the technician will take a few basic measurements. This usually involves checking your height and weight, which are essential details for comparing your results against the predicted values for someone of your size.
They’ll also ask a few questions about your medical history, any symptoms you’ve been experiencing, and the medications you take. This context helps them build a complete picture of your lung health.
Once you're settled in a comfortable chair, the main event begins. Most of the tests involve breathing into a machine called a spirometer through a sterile, disposable mouthpiece.
To make sure all the air you breathe comes from your lungs and goes directly into the machine, you’ll be asked to wear a soft clip on your nose. It might feel a bit strange at first, but it’s a simple and effective way to guarantee the readings are accurate.
Think of the technician as your personal coach throughout this process. They will give you clear, encouraging instructions for each breathing manoeuvre. Your only job is to listen carefully and give it your best shot.
Your technician’s guidance is crucial. They are trained to help you perform each breath correctly, ensuring the data collected is a true and reliable reflection of your lung capabilities.
The length of the appointment can vary. A simple spirometry test might be relatively quick, but a full set of pulmonary function tests could take anywhere from 45 to 90 minutes. This allows for crucial rest periods between the breathing efforts, which can be surprisingly tiring.
The core of the PFT involves a series of specific breathing exercises. The technician will demonstrate and explain each one before you try it yourself.
Here’s a breakdown of what you’ll likely be asked to do:
You’ll probably repeat these manoeuvres several times to ensure the results are consistent. The technician will be right there with you, cheering you on with phrases like "Keep pushing, keep pushing!" to help you get the best measurement. It’s perfectly normal to feel a bit light-headed or tired afterwards, so don’t hesitate to ask for a moment to rest.
Unfortunately, getting a diagnostic test on the NHS can sometimes mean a long wait. A 2020 report highlighted significant regional differences across England. The percentage of patients waiting six weeks or longer for a diagnostic test ranged from 22.1% in the South East to a concerning 34.4% in the North West, which can delay diagnosis and treatment. You can read the full report on NHS diagnostic waiting times for more detail.
If you’re looking to arrange a consultation or test more promptly, private options are available. You can explore how to book appointments online at The Vesey to see what is available. The entire process is designed to be as simple and stress-free as possible, giving your doctor the vital information they need to look after your health.
Getting a report filled with acronyms and numbers after a pulmonary function test can feel a bit like trying to decipher a secret code. But it’s not as intimidating as it looks. The secret is knowing that your numbers aren’t just standalone figures; they’re measured against a benchmark.
That benchmark is what we call your ‘predicted values’. These are the results a doctor would expect from a healthy person of your same age, height, gender, and ethnicity. Your results are then shown as a percentage of these predicted values, giving a clear picture of how your lungs are performing.
While the report has a lot of data, a few key measurements tell most of the story. Think of them as the main characters in your lung health narrative. Your doctor will look at how these numbers relate to each other to spot specific patterns.
Two of the most important figures you’ll see are:
The real diagnostic magic happens when we look at the relationship between these two.
This infographic gives you a simple visual of how a doctor compares predicted lung function with your actual results.
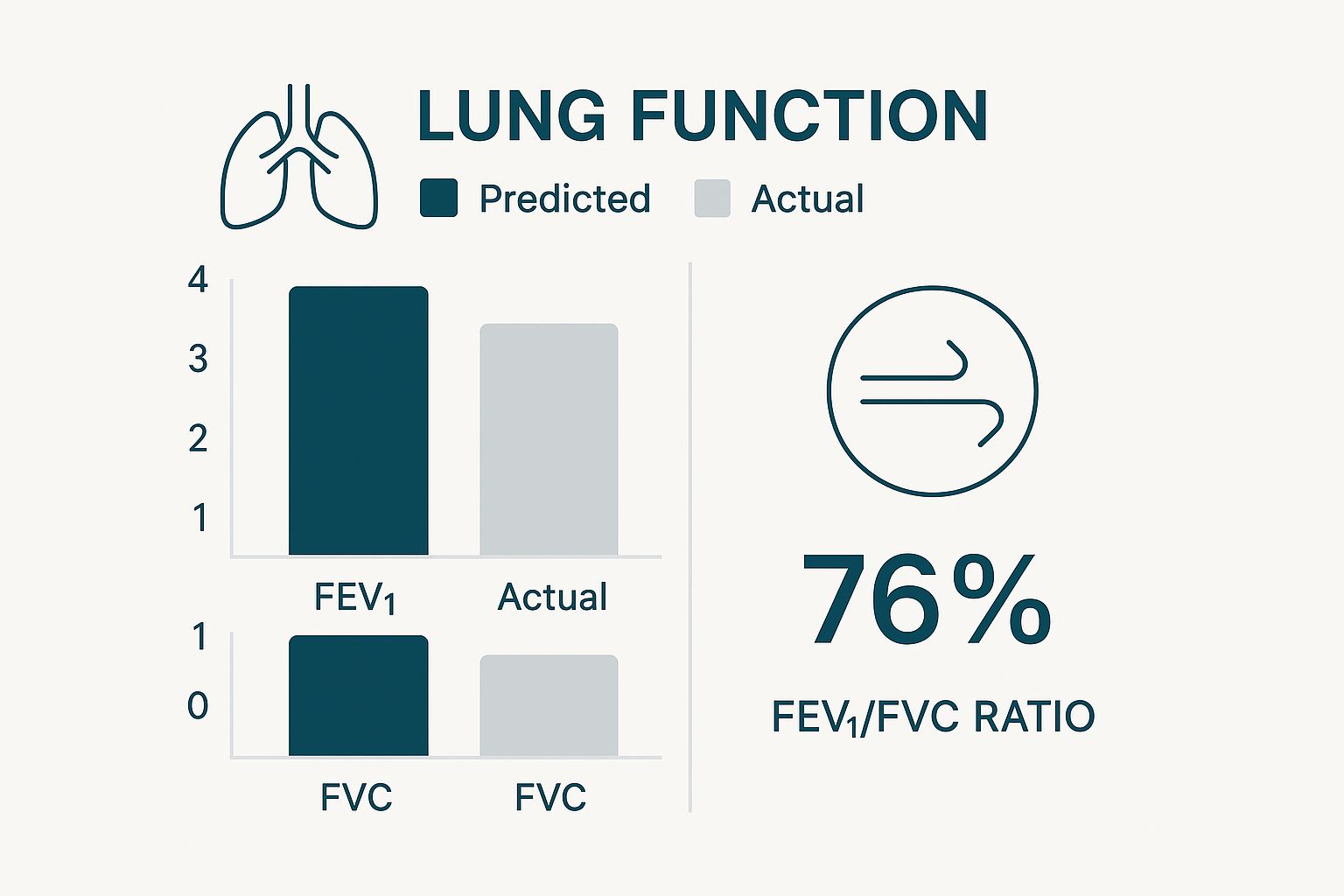
By placing the actual FEV1 and FVC values next to the predicted ones, any significant drop-off becomes immediately obvious, pointing towards a potential issue that needs a closer look.
The single most powerful tool in your PFT report is the FEV1/FVC ratio. This simple calculation—FEV1 divided by FVC—reveals an enormous amount about what’s going on inside your airways.
Think of your lungs as a full bottle of water (your FVC). The FEV1 is how much water you can squirt out in the first second. If the bottle’s opening is wide open, you’ll get a lot out fast. But if it’s narrowed or partially blocked, you’ll get much less out in that initial second, even if the bottle is completely full.
In healthy adults, you should be able to exhale around 70-80% of your total lung capacity (FVC) in that first second. This gives an FEV1/FVC ratio of 0.7 to 0.8. A ratio that’s significantly lower is a classic sign of an obstructive lung problem.
This ratio is what helps your doctor distinguish between the two main types of lung disease.
The patterns in your PFT results will generally point towards either an obstructive or a restrictive lung condition. Let’s break down what that means.
A clear way to see this is by looking at the numbers side-by-side.
Here’s a simpler way to think about it:
An obstructive pattern happens when air has trouble flowing out of the lungs, usually because the airways are narrowed. The classic sign is a low FEV1/FVC ratio (below 70%). You might be able to hold a normal amount of air, but you just can't get it out fast. This is typical for conditions like asthma and COPD.
A restrictive pattern is when the lungs themselves are stiff or can't fully expand, meaning they can’t take in a normal volume of air to begin with. Here, both your FVC and FEV1 will be lower than predicted, but the FEV1/FVC ratio is often normal or even high. Because the total lung volume is smaller, you can still empty a large percentage of it quickly. We see this in conditions like pulmonary fibrosis.
Understanding which pattern your results fit is the first step towards getting an accurate diagnosis and building the right treatment plan. If your results point to a lung condition, part of your management may involve specific exercises. You can learn more about how targeted activity helps by checking out our guide to pulmonary rehab exercises.
Your doctor will, of course, sit down with you to go over your specific results, explain exactly what they mean for your health, and talk through the next steps.

It’s completely normal to wonder about the safety of any medical test. The good news is that a pulmonary function test is overwhelmingly safe for almost everyone. It's a non-invasive procedure, which means no needles, no injections, and no radiation. The entire test just relies on your own breathing efforts.
That said, the forceful breathing required can sometimes cause a few temporary side effects. It’s not unusual to feel a bit dizzy, light-headed, or even tired during or straight after the test. This is simply your body's reaction to breathing very deeply and quickly, which can momentarily change the balance of oxygen and carbon dioxide in your blood. These feelings are brief and fade away on their own after a few moments of rest and normal breathing.
Your safety is always the number one priority. While the test itself is very low-risk, there are a few situations where your doctor might decide it's best to wait. This is purely a precaution to avoid putting any unnecessary strain on your body.
A PFT might be rescheduled if you’ve recently had:
These conditions are quite rare, and your medical team will always go through your health history thoroughly to make sure the test is right for you at this time.
A huge 20-year audit of PFTs in the UK confirms their exceptional safety record. After analysing over 186,000 tests, it found that serious complications were extremely rare, happening at a rate of roughly 1 in 10,000 tests.
This data really underscores just how routine and secure these procedures are. The study, which documented only 0.6 patient safety incidents per 1,000 tests, reported no deaths linked to PFTs, cementing their status as a standard, low-risk diagnostic tool. You can read the UK safety audit findings on PFTs for more detail. For most people, the biggest challenge is simply giving it their best effort during the breathing exercises.
To round things off, let's tackle some of the practical questions you might have swirling around in your mind. Getting straight answers can make all the difference in feeling prepared and confident for your appointment.
Not at all. A pulmonary function test is not painful. It's completely non-invasive, so there are no needles or anything that breaks the skin.
That said, it does require some real effort. You'll be asked to breathe as deeply and as hard as you possibly can, which can be tiring. Some people feel a bit light-headed or breathless for a moment afterwards, but that’s a totally normal reaction to the breathing exercises. The feeling passes very quickly once you take a moment to rest.
The raw data from the machine is ready instantly, but those numbers are just part of the story. They need an expert eye to interpret what they mean for you. A respiratory consultant will carefully review your results, considering them alongside your symptoms and medical history.
Typically, you'll go through the final, interpreted report with your referring doctor at a follow-up appointment. This way, you get a full, clear explanation of what the results mean for your health.
An abnormal PFT result isn't a diagnosis on its own. Think of it as a crucial first step, giving your doctor the objective data needed to pinpoint the cause of your symptoms and build a treatment plan that works.
Getting an abnormal result is actually a positive step—it’s the start of the journey towards the right diagnosis and treatment. The specific pattern of the results gives your doctor vital clues about what to investigate next, whether that’s an obstructive condition like asthma or a restrictive one.
From here, you might need further tests, a referral to a specialist, or you might start a new treatment plan straight away. Sometimes, breathing issues can be linked to other things, especially at night. You can learn more about how respiratory health connects with conditions like sleep apnoea from our patient resources.
Yes, absolutely. Children can have these tests, but it really depends on their age and whether they can follow the instructions. As a general rule, most children aged six and older can perform spirometry successfully.
Testing for kids involves specialised equipment scaled for smaller lung capacities. Our technicians are fantastic at coaching children through it, often turning the process into a game with plenty of encouragement to help them give their best effort and get accurate, reliable results.
At The Vesey, our dedicated respiratory team provides expert care, from accurate diagnostics to personalised treatment plans. If you have concerns about your lung health, we are here to help. Explore our services and book a consultation at https://www.thevesey.co.uk.