.webp)
Recovering from shoulder surgery isn't a quick fix; it’s a journey that unfolds in stages. While you can expect a significant healing period of three to six months, getting back to your absolute best—with full strength and mobility—can often take up to a year. It all depends on the specific procedure you've had and your body's unique healing process.
Think of your recovery timeline as a detailed road map. It’s not a sprint, but a marathon paced in distinct stages, each with its own milestones. You have to be patient and follow the route.
This guide will give you a realistic picture of what to expect, from those first few days after your operation right through to regaining full function. Your most important tools for a successful outcome will be patience and closely following the advice from your medical team. It's a partnership between you and your healthcare providers, including specialists in orthopaedic surgery.
Your recovery will be broken down into progressive phases, each with a clear focus. For instance, after a shoulder replacement in the UK, the initial recovery typically takes between three and six months. You'll likely go home with your arm in a sling, which you’ll need to wear constantly for up to six weeks to protect the delicate repairs.
Within those first six weeks, you might find you can manage simple daily tasks like dressing and washing. But remember, lifting anything heavier than a cup of tea is strictly off-limits to avoid any setbacks.
This visual guide breaks down the crucial early phases of your recovery journey.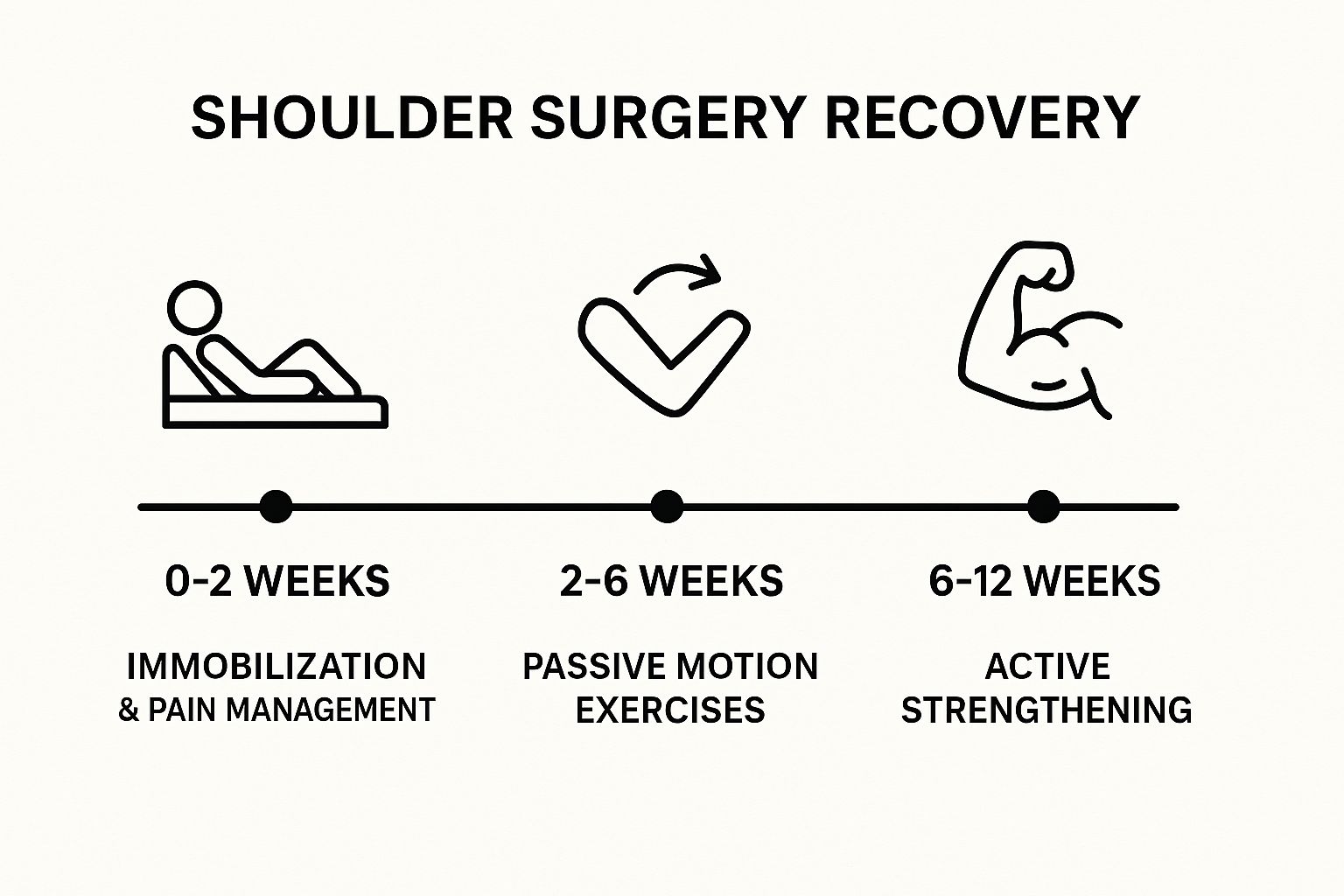
As you can see, the process moves carefully from complete immobilisation to gradually introducing gentle movements, guided by your physiotherapist, over the first three months.
The key principle behind a successful shoulder surgery recovery is progressive loading. You have to protect the repaired tissues at first, then gently challenge them to rebuild strength without causing damage. Rushing the process is the single biggest mistake people make.
Each phase is designed to build on the last, ensuring the surgical work isn't compromised. The first few weeks are all about managing pain and swelling. Next, you'll work on restoring your range of motion with assistance. Only when that solid foundation is in place can you begin the final phase: active strengthening that paves the way back to your normal life.
To give you a clearer picture, this table summarises the typical journey you can expect after shoulder surgery. It outlines what happens at each stage, how long it usually lasts, and what you'll be working towards.
Keep in mind that this is a general guide. Your personal recovery timeline will be tailored specifically to you, your surgery, and the professional advice of your surgeon and physiotherapy team.
The first six weeks after your shoulder surgery are, without a doubt, the most critical part of your recovery. Think of it like laying the foundation for a new house—it needs time to set perfectly before you can start building the walls. Your body is working overtime to heal delicate repaired tissues, and your main job is to give it the best possible environment to do so.
This means your focus needs to be laser-sharp on three things: protecting the joint, managing pain, and keeping swelling to a minimum. For this entire period, your arm will be immobilised in a sling. This isn't just a suggestion; it's a constant guardian for your shoulder, preventing any sudden movements or accidental muscle engagement that could compromise the surgeon's hard work.

Getting on top of pain is far easier than chasing it down after it’s become severe. Your surgical team will provide you with pain medication, and it's vital to follow their instructions to the letter, especially in the first few days. Taking your medication on a regular schedule, rather than waiting for the pain to spike, will keep you far more comfortable.
Ice is your other best friend during this time. Applying a cold pack to your shoulder for 15-20 minutes at a time, several times a day, is a brilliant way to tackle both swelling and pain. The cold helps constrict the blood vessels, which limits inflammation and provides a welcome numbing effect for natural relief.
It’s also worth looking into general strategies to recover muscles faster through good nutrition and sleep. A balanced diet packed with protein and vitamins gives your body the essential building blocks it needs for tissue repair.
You’ll quickly realise how many simple, everyday tasks you took for granted. Things like getting dressed, having a shower, and even eating are now logistical puzzles that require a new one-handed approach. The trick is to plan ahead.
Remember, the sling is your constant companion during this phase—even at night. It’s critical for protecting the surgical repair by stopping you from rolling onto your shoulder or moving it into a vulnerable position while you sleep.
Your active participation during what is largely a passive recovery phase is what truly sets the stage for success. While you won't be actively exercising the shoulder itself, you will likely be encouraged to do gentle hand, wrist, and elbow movements. These little motions are surprisingly important for keeping the blood flowing and preventing stiffness in the nearby joints.
Patience is paramount here. It’s easy to get frustrated by the limitations, but every single day of careful rest is an investment in your future strength and mobility. By sticking to your surgeon's protocol, you're giving your shoulder the best possible start on its journey back to full health.
For anyone undergoing a more significant procedure, understanding the full patient journey for a joint replacement can offer valuable context and help you feel more prepared. Your most important job right now is to resist the temptation to "test" your arm or rush the process. Let your body heal.
Once you hit the six-week mark, your recovery journey shifts gears into a much more active and empowering phase. The initial period of careful protection is over, and now the real work of rebuilding your shoulder begins.
Think of it this way: the first six weeks were about letting the foundation of a house set properly. Now, you can start carefully putting up the frame, piece by piece. This is where you move from passive healing to active rehabilitation.
This stage is all about your partnership with a physiotherapist. Their role is absolutely critical in guiding you as you reawaken your shoulder muscles and safely get your range of motion back. You’ll progress from gentle, passive movements—where the therapist moves your arm for you—to active-assisted and, eventually, fully active exercises.

Your first few physio sessions will focus on assessment and very gentle activation. Your therapist will check your current range of motion, pain levels, and how stable the joint is. The aim isn't to push through pain, but to gently encourage movement within a safe, comfortable range. This careful approach is key to preventing stiff scar tissue from forming later on.
The initial exercises often seem deceptively simple, but they are incredibly effective. You can expect things like:
These exercises are all designed to re-establish that mind-muscle connection and slowly improve your shoulder’s flexibility. It’s a gradual process, but every small bit of progress is a huge win.
To help you stay on track during this crucial phase, it's vital to understand what activities will help your recovery and which ones might cause a setback.
Sticking to these guidelines ensures you're helping your body heal efficiently without accidentally undoing the surgeon's hard work.
One of the most important skills you'll develop is telling the difference between "good" pain and "bad" pain. A mild stretching sensation or the ache of a muscle being worked for the first time in weeks is normal—that’s the feeling of progress. A sharp, stabbing pain, however, is a clear signal to stop.
Your body gives you constant feedback. The discomfort of rehabilitation should feel productive, like a gentle stretch, not like a warning signal. Pushing through sharp pain is counterproductive and can lead to setbacks.
Think of it like this: your physiotherapist is your guide, but your body is the map. Telling them exactly what you feel is crucial for them to adjust your programme effectively. This teamwork ensures you’re always working within your limits, which is actually the fastest route to a successful recovery. It’s also worth noting that the journey back to full function often benefits from expertise in fields like sports and exercise medicine, which can offer a broader perspective on long-term joint health.
This period is full of encouraging milestones that show you're getting your independence back. One of the biggest is graduating from your sling. Your surgeon will give you the green light to stop wearing it, usually around the six-week mark, which feels incredibly liberating.
As you progress, you'll start using your arm for light, daily activities again. Simple tasks that felt impossible before—like dressing yourself easily, carrying a light bag, or reaching for something on a low shelf—will become achievable. These small wins are fantastic morale boosters.
By the end of this phase, you’ll still be avoiding heavy lifting or sudden, forceful movements. However, your shoulder should feel significantly more mobile and useful. You're building the essential foundation of flexibility and muscle control that is vital for the next stage: building serious strength.
Hitting the three-month mark is a huge milestone in your recovery. It’s where the focus really shifts from gently coaxing back your range of motion to actively building real, functional strength. All that hard work you've put in with your physio is about to pay off in a big way, clearing the path back to a full and active life.
Think of the first few months as learning the individual notes on an instrument. Now, you’re finally ready to start stringing them together to play actual songs. Your physiotherapist will start introducing a new set of strengthening exercises, probably using resistance bands, light weights, and bodyweight movements. These are all designed to safely challenge your shoulder muscles and rebuild what was lost.
Consistency is everything at this stage. The aim is to progressively overload the muscles, encouraging them to get stronger week after week. Each session builds on the one before, slowly preparing your shoulder for the demands of everyday life and, eventually, much more.
As you feel your strength and confidence returning, you can start reintroducing more of your usual activities. It’s an exciting time, but you still need to be sensible and measured. Always have a chat with your surgeon and physiotherapist before making any major leaps.
Here’s a rough idea of what to expect when returning to some key activities:
The quality of your surgical care plays a massive role in these long-term outcomes. For instance, a UK study involving over 39,000 patients found that those treated by surgeons who perform more than 10 shoulder replacements a year had better results and were less likely to need another operation down the line. It just goes to show how much specialist experience matters. You can read more about these surgical outcome findings to see why that expertise is so important.
While you'll feel a world away from where you started by the six-month point, it's crucial to remember that full recovery is a marathon, not a sprint. You’ll continue to see subtle improvements in your strength, coordination, and stamina for up to a year, and sometimes even longer.
Your shoulder hasn't just been repaired; it has learned a completely new way of moving. It takes time for your brain and muscles to perfect this new partnership, which is why you'll keep noticing small gains long after the initial healing is done.
This final stretch is incredibly rewarding. You’ll start noticing little victories, like reaching for something on a high shelf without a second thought or sleeping soundly on your operated side. For those looking at ways to support joint health in the long run, it can be beneficial to explore treatments that aid tissue repair. Our detailed guide explains how therapies like PRP for joints are used to support the body’s natural healing processes.
Patience is still your best friend. Celebrate every bit of progress, stick with your physiotherapy exercises, and always listen to your body. You've already navigated the toughest parts of this journey. The strength you’re building now is the key to reclaiming the active, pain-free life you’ve worked so hard for.

While the recovery timelines we've looked at offer a solid map, it’s vital to remember they are just a guide. Your personal shoulder surgery recovery is as individual as you are. Think of it like training for a marathon; everyone follows a similar plan of building up mileage and strength, but each runner’s progress is shaped by their own body, preparation, and dedication.
A few key variables come together to create your unique recovery experience. Some of these are completely out of your hands, determined by the specifics of your surgery and your personal health. But thankfully, many powerful factors are firmly within your influence, letting you play an active role in how well and how quickly you heal.
Understanding the fixed elements of your recovery helps set realistic expectations right from the start. These factors create the baseline for your healing journey.
It's also worth noting just how common these procedures are becoming. Data from England shows a significant rise in shoulder replacements, with 6,281 performed in 2019. Projections suggest this could increase by a staggering 234% to over 20,900 by 2050. You can explore the full financial and healthcare implications of these trends in this detailed analysis of NHS surgical data.
This is where you can truly make a difference. The choices you make before and after your operation have a massive impact on your final outcome.
Your surgeon performs the repair, but you are the one who performs the recovery. The single biggest factor in your success is your commitment to the rehabilitation process.
Let's break down the key areas where your efforts will pay the greatest dividends:
By understanding these variables, you can better navigate the ups and downs of healing. While you can't change the type of surgery you need, you can control your diet, your lifestyle, and your dedication to the rehab plan. For anyone dealing with ongoing joint issues, learning more about the causes and treatments for musculoskeletal pain can provide valuable context. Embracing your active role is the key to achieving the best possible outcome.
As you get into the swing of your recovery, it’s completely normal for practical, everyday questions to come up. Think of this section as a quick reference guide, put together to answer some of the most common things we get asked, helping you navigate your healing with a bit more confidence.
This is a big one. For most people, trying to sleep flat in a normal bed is just too uncomfortable for the first four to six weeks. The position puts a lot of pressure on the healing shoulder, which can lead to a lot of pain and a restless night.
Many of our patients find that sleeping in a recliner is the best option initially. If you don't have one, propping yourself up in bed with a good number of pillows can work just as well. This elevated position is key to keeping pain and swelling down. And remember, you absolutely must keep your sling on while sleeping during this phase to protect the repair work. Once your surgeon gives you the green light, you can start the gradual transition back to your bed.
Knowing what to look for is crucial for a safe and smooth recovery. It's important to get in touch with your doctor straight away if you spot any of these potential signs of an infection or other issues.
Keep an eye out for these red flags:
Catching these problems early makes all the difference. Never hesitate to seek medical advice if something feels off.
You'll need to have a direct conversation with your surgeon about this one. As a general rule, a short flight might be manageable after a few weeks, but we strongly advise against any long-haul travel for at least six to eight weeks.
The main worries are the heightened risk of blood clots (deep vein thrombosis) from sitting still for so long, and simply how difficult it is to stay comfortable while protecting your shoulder in a cramped airline seat. Always get explicit clearance from your surgical team before you even think about booking a flight.
"Your active participation is just as important as the procedure itself. The surgery repairs the joint, but the exercises are what rebuild your strength, motion, and function."
To put it simply: no. Your physiotherapy programme is the absolute cornerstone of a successful recovery. While the surgeon has masterfully repaired the joint, it’s the consistent, dedicated work you do in physio that retrains the muscles and gets your shoulder working properly again.
Skipping exercises or being inconsistent is one of the main reasons for a poor outcome. It often leads to lasting stiffness, weakness, and drags out your overall shoulder surgery recovery time. While exploring the medical and healing applications of complementary therapies can be part of a holistic approach, these should only ever be considered as a supplement to, never a replacement for, the core rehabilitation plan your physiotherapist has prescribed.
At The Vesey, our dedicated team of orthopaedic specialists and physiotherapists is committed to guiding you through every stage of your recovery. We provide expert, personalised care to ensure you achieve the best possible outcome. Learn more about our comprehensive orthopaedic services at https://www.thevesey.co.uk.

