.webp)
It’s a fact of life: testosterone levels don't stay the same forever. They hit their peak in our late teens and early twenties, and from there, it's a gradual, gentle decline. For men here in the UK, what's considered "normal" is a pretty broad range, typically sitting between 8.7 to 29 nmol/L. But this is a moving target, shifting quite a bit as we move through different stages of life.
Trying to understand your testosterone levels isn't about chasing one magic number. It’s more about recognising that your body is on a lifelong journey. Think of it like a car. When it's new, the engine is powerful and responsive. Over the years, that peak performance naturally tempers, and it needs a bit more care to keep running smoothly.
Your hormonal health is no different. That incredible energy and physical prime you feel in your 20s is fuelled, in large part, by high testosterone. But that's just the starting point of a long, gentle curve, not a permanent state.
The thought of declining hormones can sound a bit unnerving, but it’s a completely normal part of ageing. This isn't a sudden cliff-edge drop; it's a slow and steady adjustment year after year. That's why most men don't notice any drastic changes from one birthday to the next.
Over a decade, however, the cumulative effect can become more obvious. The trick is to know what’s typical for your age group, which helps you set realistic expectations for your health, energy, and overall well-being. This knowledge is empowering, helping you tell the difference between standard ageing and something that might need a closer look.
Your body’s hormonal clock doesn't just stop; it winds down gracefully. Knowing the expected testosterone levels by age helps you listen to what your body is telling you, ensuring you can provide the right support at the right time.
Take UK men, for example. Research shows the trend very clearly. Lads aged 20-24 typically have total testosterone levels between 14.2 and 19.3 nmol/L. Fast forward to their early 40s, and that range has shifted down to between 12.1 and 16.4 nmol/L. This lines up perfectly with the well-documented pattern of a roughly 1% decline per year after 30. You can learn more about these age-specific findings and see how UK men compare.
It’s crucial to understand that there isn’t one single "normal" number for testosterone. Instead, think of it as a sliding scale that naturally adjusts as you move through different stages of life. What’s optimal in your twenties is very different from what’s typical in your sixties.
Let’s explore what these typical ranges look like decade by decade. This will give you a much clearer picture of the body's natural hormonal rhythm, from the peak years of young adulthood to the more noticeable shifts later in life.
This data gives a great visual overview of the average decline in testosterone levels from the 20s right through to the 60s.
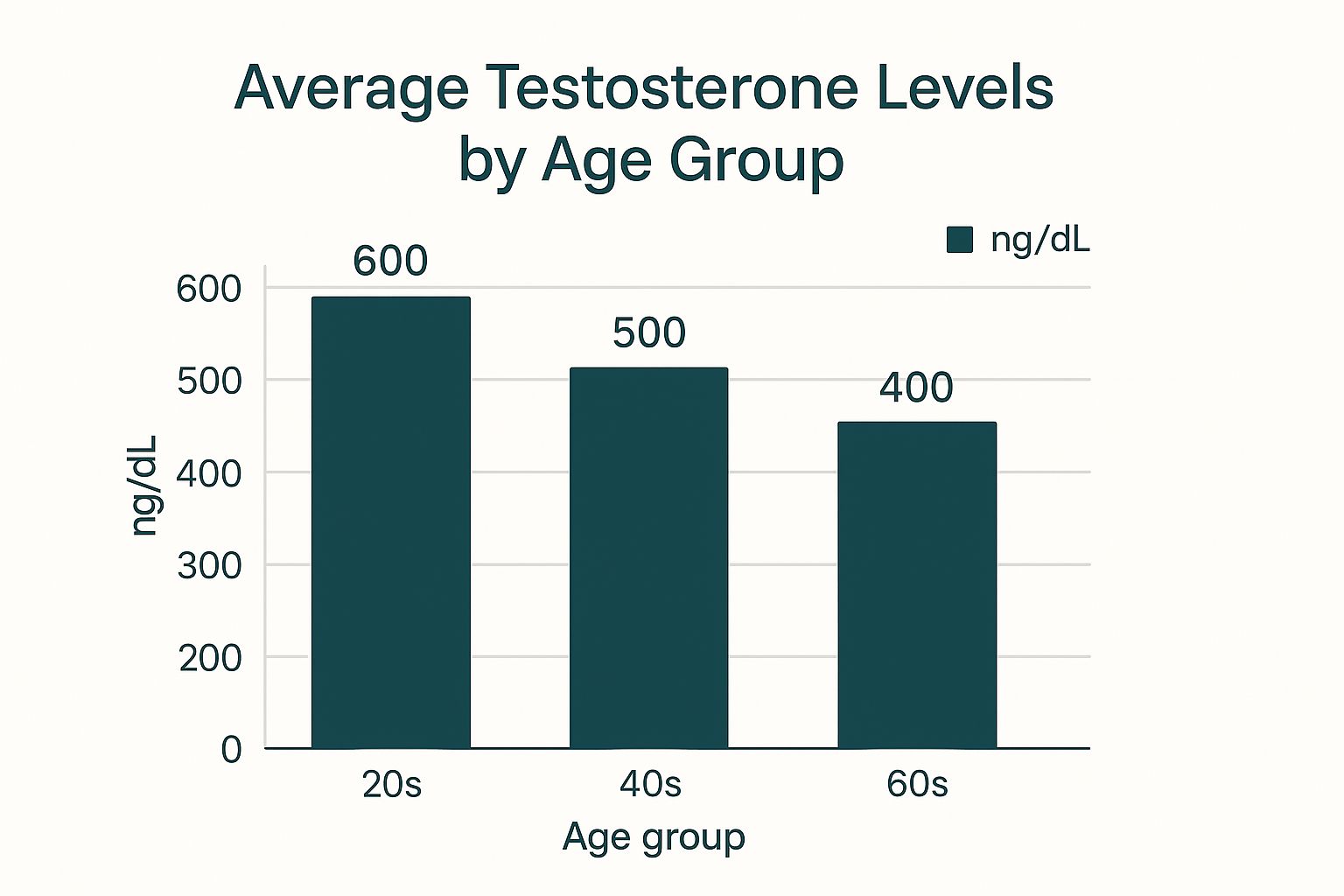
As you can see, there's a steady, predictable drop in average testosterone with each passing decade.
To put this into context, here’s a table outlining the typical ranges and their roles at each stage.
This table shows the approximate normal ranges for total testosterone in nanomoles per litre (nmol/L) for different age groups, reflecting the natural decline over time.
These figures provide a helpful benchmark, but remember that individual health, genetics, and lifestyle play a massive part in where you might fall within these ranges.
In your twenties, your body is essentially a testosterone-producing powerhouse. Levels are at their lifetime high, fuelling everything from muscle growth and bone density to your energy and sex drive. This is the biological foundation for building the strength and vitality that will support you for years to come.
It's not just about the 'total' testosterone in your bloodstream, which is high. Just as importantly, the 'free' testosterone—the portion your body can actually put to work—is also abundant. This is why physical recovery often feels faster and building muscle seems easier during this decade.
Around the age of 30, a slow and steady decline begins. On average, this happens at a rate of about 1% per year. The change is so gradual that most men simply don't notice it in their day-to-day lives.
However, over the course of these two decades, the cumulative effect can start to surface. You might find that maintaining muscle mass requires a bit more effort, or that your energy levels aren't quite what they used to be. This isn't a sign of a problem; it’s just the natural progression of hormonal ageing.
Understanding this natural decline is crucial. It helps you differentiate between normal ageing and symptoms that might warrant a conversation with a doctor. A proactive approach allows you to support your body effectively through every stage of life.
A comprehensive check-up can give you a clear snapshot of where your health markers stand. To get a detailed picture, consider exploring an essential health assessment, which provides invaluable insights into your overall well-being.
By the time you hit your 50s, 60s, and beyond, the decline in testosterone is more established. The average levels are noticeably lower than in your younger years, and the physical signs of this shift can become more apparent.
Common experiences include:
It’s vital to remember that these are just general trends. An individual’s testosterone level can vary widely based on genetics, lifestyle, and overall health. Knowing the typical testosterone levels by age provides a useful benchmark, but it’s certainly not a rigid rule.
Knowing your total testosterone number is useful, but it's only one piece of the puzzle. The real story is about how much of that hormone your body can actually use. This is where a critical protein called Sex Hormone-Binding Globulin (SHBG) comes into play, acting as the main regulator of your available testosterone.
Think of SHBG as a fleet of secure transport vehicles in your bloodstream. Their primary job is to bind to testosterone, effectively locking it up and taking it out of circulation. This is a perfectly normal and necessary process, but it's the balance between this "bound" testosterone and "free" testosterone that truly impacts how you feel.
As men age, the body naturally starts to produce more of these SHBG vehicles. This means a larger chunk of your total testosterone gets bound up and becomes unavailable for your cells to use. It’s a subtle but powerful shift that explains why two men with the exact same total testosterone level can experience completely different symptoms.
The hormone that isn't bound to SHBG is called free testosterone. This is the active, bioavailable form that can get into your cells and do all the important things we associate with testosterone – from building muscle and bone density to maintaining your mood and libido.
Because SHBG levels tend to creep up with age, the amount of free testosterone often drops off more steeply than total testosterone. This is a crucial detail for getting a complete picture of your hormonal health, particularly as you get into your 40s, 50s, and beyond. Taking a closer look at your own reproductive health can shed light on how all these moving parts are working together.
It’s not just about the total amount of fuel in the tank (total testosterone), but how much of that fuel can actually get to the engine (free testosterone). Rising SHBG levels can effectively pinch the fuel line, even if the tank seems full.
On top of the long-term changes that happen over your lifetime, testosterone also follows a daily rhythm, known as a diurnal cycle. For most men, levels are highest first thing in the morning and then gradually fall throughout the day, hitting their lowest point in the evening.
This daily swing is most noticeable in younger men. For instance, men under 40 might see their testosterone levels fluctuate by as much as 30-35% between their morning peak and their afternoon low. This is precisely why doctors always recommend a morning blood test to get the most accurate and reliable reading.
As you get older, however, this daily rhythm tends to flatten out. While your overall testosterone might be declining by about 3% to 10% per decade after you hit your 20s, the daily variation also shrinks, dropping to around 10% by the time you're 70. This blunted cycle, combined with the steady rise in SHBG, is a key part of the hormonal changes that come with ageing. Discover more insights about what determines normal testosterone levels on balancemyhormones.co.uk.
While it's true that testosterone levels naturally dip as we get older, your daily habits and choices have a massive say in how fast that decline happens. It's a bit like being given a car – your genetics are the model you start with, but your lifestyle is how you drive and maintain it. Bad habits can accelerate the wear and tear, but good ones can keep the engine running smoothly for years to come.
Your day-to-day routine, from the food on your plate to how you handle stress, directly fiddles with your hormonal thermostat. This isn't just an age thing; it's about the environment you create for your body to thrive in.
Chronic stress is one of the biggest enemies of healthy testosterone. When you're constantly on edge, your body floods itself with a hormone called cortisol. The easiest way to think about it is to picture a seesaw: when cortisol goes up, testosterone often goes down.
This happens because cortisol puts your body into "fight or flight" mode. In this state, things like reproduction and muscle-building are put on the back burner. They're considered non-essential when survival is the priority, so the resources needed for testosterone production get diverted. Over time, persistently high cortisol can actively suppress your body's ability to make testosterone.
Your body composition has a direct and powerful impact on your testosterone. Excess body fat, especially around your middle, contains an enzyme called aromatase. This enzyme has one job: to convert your precious testosterone into oestrogen, which effectively robs you of the testosterone you have.
The good news? You can fight back with one of the best tools in the box: resistance training.
Getting a regular exercise routine going is one of the most significant changes you can make. You can learn more about the extensive benefits of exercise in our detailed guide.
Lifestyle isn't a minor detail; it's a central pillar of hormonal health. Simple, consistent changes in diet, exercise, and stress management can make a noticeable difference in maintaining healthy testosterone levels as you age.
Interestingly, these lifestyle factors can even lead to regional differences in average testosterone levels across the UK. For instance, men in London, which has a younger average population, recorded the highest average levels at 17.2 nmol/L. At the other end of the scale, the North East, with an older demographic, showed the lowest at 15.9 nmol/L. Researchers point to a mix of factors like diet, stress levels, and overall lifestyle choices to explain this gap.
Diet is, of course, a huge piece of the puzzle. Your body needs specific building blocks to produce testosterone efficiently. The key players include:
For anyone looking to be proactive about their hormone health, getting a handle on these natural methods is a great place to start. You can explore a detailed guide on natural ways to boost testosterone. By focusing on the factors you can actually control, you give your body the best possible chance to maintain its hormonal health, no matter your age.

While knowing the numbers behind testosterone levels by age is a good starting point, it’s the real-world impact that you’ll actually feel. Learning to spot the signs of low testosterone (often called "low T") is the first step toward having a productive conversation with your doctor about how you’re feeling.
The tricky part is that these symptoms often creep up on you. They can easily be brushed off as just the side effects of a stressful life or the natural process of getting older.
To make things clearer, it helps to think of the potential signs in three main categories: physical, sexual, and emotional. This makes it much easier to connect the dots.
The physical signs of low T often show up as changes to your body composition and overall energy. Testosterone is central to maintaining muscle and bone, so when your levels dip, you’ll likely notice it.
You might be experiencing things like:
These symptoms alone aren't definitive proof of low testosterone. But if you're noticing a consistent pattern, it's something to pay close attention to.
This is probably the most well-known area affected by low testosterone. Testosterone is the main driver of male libido, so it's no surprise that a decline can directly affect your sex drive and performance.
It's crucial to remember that symptoms like a low sex drive can have many causes, including stress, relationship issues, or other medical conditions. Low testosterone is just one possibility on a longer list.
The key signs to look for are a noticeably lower interest in sex (low libido) and trouble getting or maintaining an erection. Low T can also affect fertility, since testosterone is vital for producing sperm. If this is a concern, you can find helpful information on male infertility and its causes.
Testosterone's influence goes beyond the purely physical—it also affects your mood and mental sharpness. A hormonal imbalance can sometimes appear as emotional or cognitive struggles that are hard to put your finger on.
These shifts might include:
The goal here isn't to self-diagnose. It’s about gathering information. When you can walk into your GP's office with specific concerns, you’re setting yourself up for a much more focused and productive conversation about your health.
https://www.youtube.com/embed/UpGKPTLOmIo
If you're grappling with symptoms and think low testosterone might be the cause, the first port of call is usually a chat with your GP. This is your chance to lay out exactly what you've been experiencing, giving your doctor the full picture needed to decide if a blood test is the right next step.
When it comes to the test itself, timing is everything. Testosterone levels naturally ebb and flow throughout the day, hitting their peak in the morning. That’s why any blood test for testosterone should be done before 10 a.m. to get an accurate reading. An afternoon test can show a falsely low number, which is why a morning appointment is standard procedure.
Here in the UK, you generally have two routes for getting your hormone levels checked: through the NHS or with a private clinic. The NHS will usually greenlight a test if you’re showing clear clinical symptoms, whereas private clinics can offer more direct and immediate access to comprehensive hormone panels.
A single blood test is rarely the final word. It's just a snapshot in time. To confirm a diagnosis of low testosterone, doctors will almost always ask for at least two separate morning readings to make sure the result is consistent and not just a one-off dip.
A full hormone panel offers a far more detailed story than just a single testosterone figure. It typically looks at levels of SHBG, albumin, and other crucial related hormones. For those keen to get moving, exploring your options for private blood testing can be a quicker way to get the detailed insights you’re looking for.
For even more convenience, you might also consider Hormone Level Testing at Home, which offers another practical way to gather crucial data about your hormonal health from your own home.
As we wrap up our deep dive into testosterone levels, you might still have a few things on your mind. That's perfectly normal. Let's tackle some of the most common questions we hear, giving you clear, straightforward answers to round out your understanding.
Think of this as the final piece of the puzzle, designed to clear up any lingering myths and give you total confidence in managing your hormonal health.
Absolutely. Making smart lifestyle changes can have a surprisingly powerful effect on your body's hormone production. You don't need to do anything drastic; simple, consistent habits are often the best tools for the job.
Here are the cornerstones of naturally supporting your testosterone:
While these strategies are fantastic for optimising healthy levels, it’s important to remember they might not be enough to fix a clinically diagnosed deficiency on their own.
When it's prescribed and managed by a qualified doctor for a genuine medical need, Testosterone Replacement Therapy (TRT) is generally considered a safe and effective treatment. Before anyone starts, a thorough health screening is always carried out to make sure it's the right and safe choice for them.
The key to safety with TRT is proper medical supervision. Regular blood tests are vital to track your hormone levels, catch any potential side effects early, and ensure your dose is perfectly optimised for you.
Trying to self-prescribe or using unregulated products you find online is incredibly dangerous and comes with serious health risks. This is something you must do with a healthcare professional.
The supplement market is flooded with products making big promises, but the reality is often less impressive. It's a mixed bag, to be honest. Some supplements contain genuinely useful nutrients like zinc or vitamin D, which can certainly help if you're deficient in them.
However, many of the so-called "T-boosters" are packed with herbal ingredients that just don't have the strong scientific backing to prove they can meaningfully raise testosterone. Before you start taking any new supplement, it's always a good idea to have a chat with your doctor. Focusing on getting your nutrients from a well-rounded diet is always the best place to start.
At The Vesey, we believe everyone deserves clear, expert guidance on their health journey. If you're concerned about your hormone levels or any other aspect of your well-being, our specialists are here to provide exceptional, personalised care. Learn more about our services and see how we can support you.

