.webp)
If you’re wondering, “Why do I keep getting thrush?”, you’re definitely not alone. It's a frustrating cycle, but one thing is clear: this isn’t about hygiene. Almost every case of recurrent thrush comes down to an internal imbalance that turns your body into an environment where yeast can thrive over and over again.
Getting to the bottom of what is disrupting this delicate balance is the first real step toward breaking the cycle for good.
Thrush is incredibly common—around 75% of women will have it at least once. But for a smaller group, it becomes a persistent, recurring problem.
This is officially known as recurrent vulvovaginal candidiasis (RVVC), which means having four or more diagnosed episodes within a single year. Research shows this affects about 5% of women, highlighting just how relentless this condition can be for some.
So, what turns a one-off infection into a repeating nightmare? Think of your body’s natural microbiome as a well-kept garden. Normally, beneficial bacteria (the 'good guys') keep the naturally present Candida yeast (the 'weeds') in check. Recurrent thrush happens when something keeps disturbing the garden, letting the weeds overgrow again and again.
Several factors can upset this delicate ecosystem, leaving you vulnerable to frequent infections. Pinpointing these is key to understanding your personal triggers.
By looking beyond the immediate symptoms and digging into these deeper influences, you can start to piece together the puzzle. Our detailed guide on the various causes of thrush can offer even more insight into what might be triggering your episodes.
If you're stuck asking, "why do I keep getting thrush?", the answer usually isn't just one thing. It's often a handful of key triggers that repeatedly knock your body's natural balance off-kilter. Think of these culprits as the blueprints for the cycle of infection; once you identify them, you can start to break that cycle down.
These triggers are often tangled up with each other, creating the perfect storm for yeast to take over. The infographic below shows how major factors like antibiotics, hormonal shifts, and your immune system’s strength are all connected to this internal imbalance.
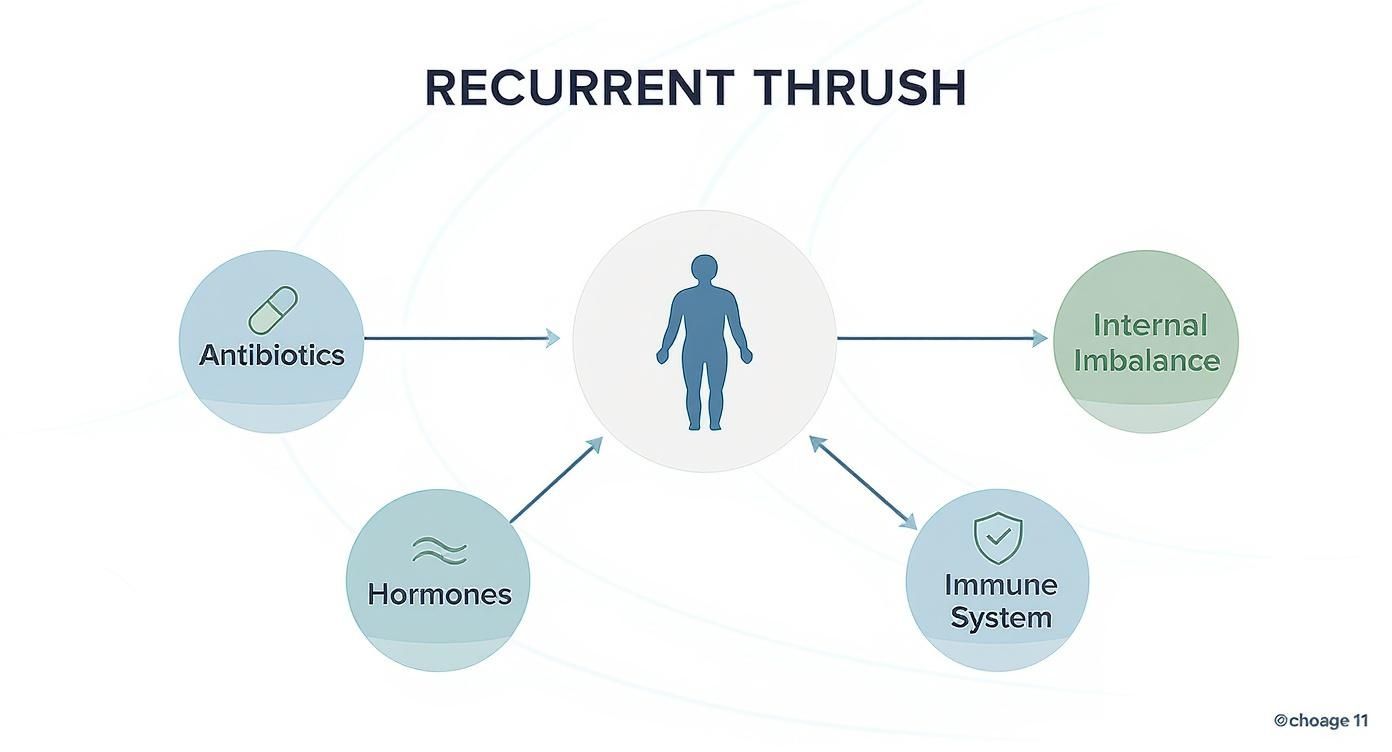
As you can see, what’s happening inside your body has a direct impact on how susceptible you are to thrush. It's rarely down to one isolated cause. Let’s take a closer look at these hidden drivers.
Broad-spectrum antibiotics are a massive—and very common—cause of recurrent thrush. While they're brilliant at fighting off nasty bacterial infections, they don’t really distinguish between 'good' and 'bad' bacteria.
Imagine it like using a powerful weed killer that also wipes out all the beneficial plants in a garden. By killing off protective bacteria like Lactobacillus, antibiotics leave a wide-open field for Candida yeast to grow without any competition.
This is exactly why so many women find themselves with a thrush infection either during or right after finishing a course of antibiotics.
Your hormones, especially oestrogen, play a huge role in keeping the vaginal environment balanced. When oestrogen levels climb, they can actually encourage yeast to grow and attach more easily to the vaginal walls.
These hormonal shifts are a perfectly normal part of life, but they create windows of opportunity for thrush to strike.
Sometimes, recurrent thrush is less of a standalone issue and more of a signpost pointing to a deeper health problem that needs sorting out. An imbalanced internal system is the ideal breeding ground for yeast.
Uncontrolled high blood sugar is a major contributor to recurrent thrush. Yeast loves sugar, and having too much of it in your system is like laying out an endless buffet for Candida to feed on and multiply.
This is particularly true for diabetes. The risk of getting thrush again and again is higher in women with certain risk factors, and those with poorly managed diabetes are up to three times more likely to develop recurrent thrush.
If you have any concerns about your blood sugar, looking into your diabetes status can be a crucial first step. It's not just about the sugar you eat, either. Your body's response to certain foods can be a hidden trigger; understanding what causes insulin spikes can show how different dietary choices might be making you more susceptible.
On top of that, any condition that weakens your immune system—whether it’s chronic stress or an illness—lowers your body's ability to keep Candida in check, leaving you much more vulnerable to repeated infections.
To help put this all into perspective, here’s a quick summary of the main triggers we’ve covered.
Understanding how these factors work is the first real step towards managing the problem for good, rather than just treating the symptoms as they appear.
Beyond clear medical causes, some of your daily routines might be unknowingly creating the perfect conditions for thrush to thrive. If you're constantly asking, "why do I keep getting thrush?", it’s worth taking a closer look at your everyday habits. You might find some surprising connections.
Even small, seemingly harmless choices can add up, disrupting your body's delicate balance and making you more susceptible to those frustrating, recurrent infections.

The link between what you eat and yeast overgrowth is often debated, but the science is pretty straightforward: Candida yeast feeds on sugar. Now, a single chocolate bar won't instantly trigger a flare-up, but a diet consistently high in refined sugars and carbohydrates can certainly help create an environment where yeast flourishes.
This doesn't mean you need to banish all sugar from your life. It's more about being mindful of your intake as a powerful preventative step. If you're concerned about how your diet might be affecting your overall health, a comprehensive lifestyle screen can offer valuable insights into your body's unique needs.
Believe it or not, your wardrobe could be a bigger factor than you realise. Yeast loves warm, damp, and dark environments, and certain types of clothing create exactly that.
Simple swaps can make a huge difference. Opting for looser-fitting clothing and choosing natural, breathable fabrics like cotton for your underwear helps keep the area dry and cool. It makes it a much less hospitable place for yeast to set up camp.
A common misconception is that more aggressive cleaning equals better hygiene. In reality, harsh or perfumed products can do more harm than good, stripping away the protective bacteria that keep yeast in check.
Many well-intentioned hygiene practices can ironically increase your risk of thrush. How? By disrupting the vagina's natural pH balance. The vaginal environment is clever – it's self-cleaning and relies on a delicate ecosystem of bacteria to stay healthy.
Try to avoid these common culprits:
By making these small but meaningful adjustments to your daily habits, you can help restore your body's natural defences and create an environment that actively discourages thrush from coming back.
https://www.youtube.com/embed/s8ORMwF-HHE
If you find yourself constantly asking, “why do I keep getting thrush?”, you know the frustrating ritual of reaching for the same over-the-counter cream all too well. While these treatments might offer some temporary relief, they don’t get to the heart of the problem.
When thrush becomes a recurring visitor, self-diagnosing is rarely enough to break the cycle for good. Securing a professional diagnosis from your GP is the most important first step. The classic symptoms—itching, soreness, and unusual discharge—can easily be confused with other common conditions. What feels like another bout of thrush could actually be something else entirely.
Getting the right diagnosis is essential because the treatment for one condition won't work for another and could even make things worse. Several other issues present with very similar symptoms, which is where a lot of the confusion comes from.
To get a clear picture of what’s really going on, your GP may suggest taking a small swab from the affected area. It’s a simple, painless test, but it’s incredibly valuable. It will definitively confirm whether Candida yeast is the culprit behind your symptoms, putting you on the right path to effective treatment.
A swab test does more than just confirm a yeast infection. It can identify the specific strain of Candida causing the problem, which is vital for effective treatment, especially in recurrent cases.
Most thrush infections are caused by a strain called Candida albicans, which usually responds well to standard antifungal treatments. But every now and then, a different, more resistant strain is to blame. Surveillance from the UK Health Security Agency has even noted a slight rise in serious yeast infections, including emerging pathogens like Candida auris that can cause difficult-to-treat infections. You can learn more about these public health findings from their official report.
Identifying a less common strain allows your doctor to prescribe a more targeted and effective treatment plan. This is often the key to finally breaking free from the frustrating cycle of recurrence.
When you’re stuck in a loop of recurrent thrush, a single-dose cream from the chemist often feels like putting a tiny plaster on a much bigger problem. It might offer temporary relief, but it rarely gets to the root of why it keeps coming back. To truly break the cycle, we need a far more structured and strategic medical approach.
This means shifting your mindset from just treating the symptoms as they pop up to creating a long-term plan. The goal isn’t just to clear the current infection, but to actively prevent the next one from ever getting a foothold. It's about moving from reactive fixes to proactive management.
An effective medical strategy for recurrent thrush is nearly always broken down into two distinct phases. This ensures we deal with the immediate problem head-on before putting strong preventative measures in place.
This two-pronged attack is crucial. Recurrent thrush often involves a more established colony of yeast that a simple one-off treatment just can’t fully eradicate.
A plan tailored by your GP will go far beyond standard over-the-counter options. Because recurrent cases are tougher, they almost always require stronger or more prolonged treatment to work.
For the initial induction phase, this could involve:
After that, maintenance or suppression therapy is the real key to long-term relief. This is a preventative strategy that continues for several months, sometimes longer.
Suppression therapy is the cornerstone of managing recurrent thrush. It typically involves taking a low-dose oral antifungal tablet or using a pessary just once a week for up to six months. This approach doesn't aim to wipe out Candida completely but to keep its population so low that it no longer causes any symptoms.
This long-term plan helps restore and maintain the natural balance of your vaginal microbiome, giving your body the space it needs to regain control. It’s a marathon, not a sprint, but it’s designed to finally stop that frustrating cycle of infection and reinfection.
It’s vital to have an open conversation with your GP to create a structured plan that’s right for you. They can help diagnose the specific cause and rule out other issues, such as different vulva conditions that can sometimes mimic thrush symptoms. By working together, you can develop a medical strategy that finally puts you back in control.
Breaking the cycle of recurrent thrush isn’t about drastic overhauls. It’s about making small, consistent changes that help restore and protect your body’s natural balance. Think of it as your personal toolkit for taking back control.
This action plan pulls together the most effective strategies into simple, daily habits. By putting these into practice, you can significantly reduce your risk of future flare-ups and finally get an answer to that frustrating question: "why do I keep getting thrush?".
The environment you create down there matters, a lot. Yeast loves warm, moist conditions, so improving air circulation is one of the simplest yet most powerful things you can do.
When it comes to vaginal health, gentle care is far more effective than aggressive cleaning. In fact, harsh products can strip away the protective bacteria that keep your vaginal microbiome in balance. Your body has a brilliant self-cleaning system; your job is to support it, not disrupt it.
One of the most common mistakes I see is over-cleaning with harsh or perfumed products. This can disrupt the delicate vaginal pH, ironically making you more susceptible to the very infections you're trying to prevent.
To protect this delicate balance, stick to these simple rules:
When you're dealing with thrush that just won't go away, it’s natural to have a lot of questions. Let's tackle some of the most common ones that come up.
This is a really common worry, but it's usually not the case. While it's technically possible to pass yeast between partners during sex, thrush isn’t classed as a sexually transmitted infection (STI). For most women, the real culprit is an internal imbalance in their own body, not something they've caught.
However, if your partner is showing symptoms themselves (like redness or irritation), treating both of you at the same time can sometimes help break a frustrating cycle of reinfection.
There’s a lot of buzz around probiotics, and for good reason. Certain probiotic supplements containing specific strains of Lactobacillus bacteria can help support a healthy vaginal microbiome, which is your body’s first line of defence against yeast overgrowth.
Some women find them particularly useful when taking a course of antibiotics, which can disrupt that delicate balance. The science is still growing in this area, so it’s always a good idea to chat with your GP to see if probiotics are a good fit for you.
Yes, it absolutely can be a factor. Chronic stress puts your immune system under pressure, making it less effective at keeping the naturally present Candida yeast under control.
While stress on its own is rarely the single cause of recurrent thrush, it can certainly lower your defences and make you more vulnerable to a flare-up. Managing stress through things like regular exercise, mindfulness, or simply prioritising a good night's sleep can give your immune system the support it needs to fight back.

